Corpus: Prostate
from ancient Greek: προστάτης ("prostátēs") - prostate
Synonym: prostate gland
1. Definition
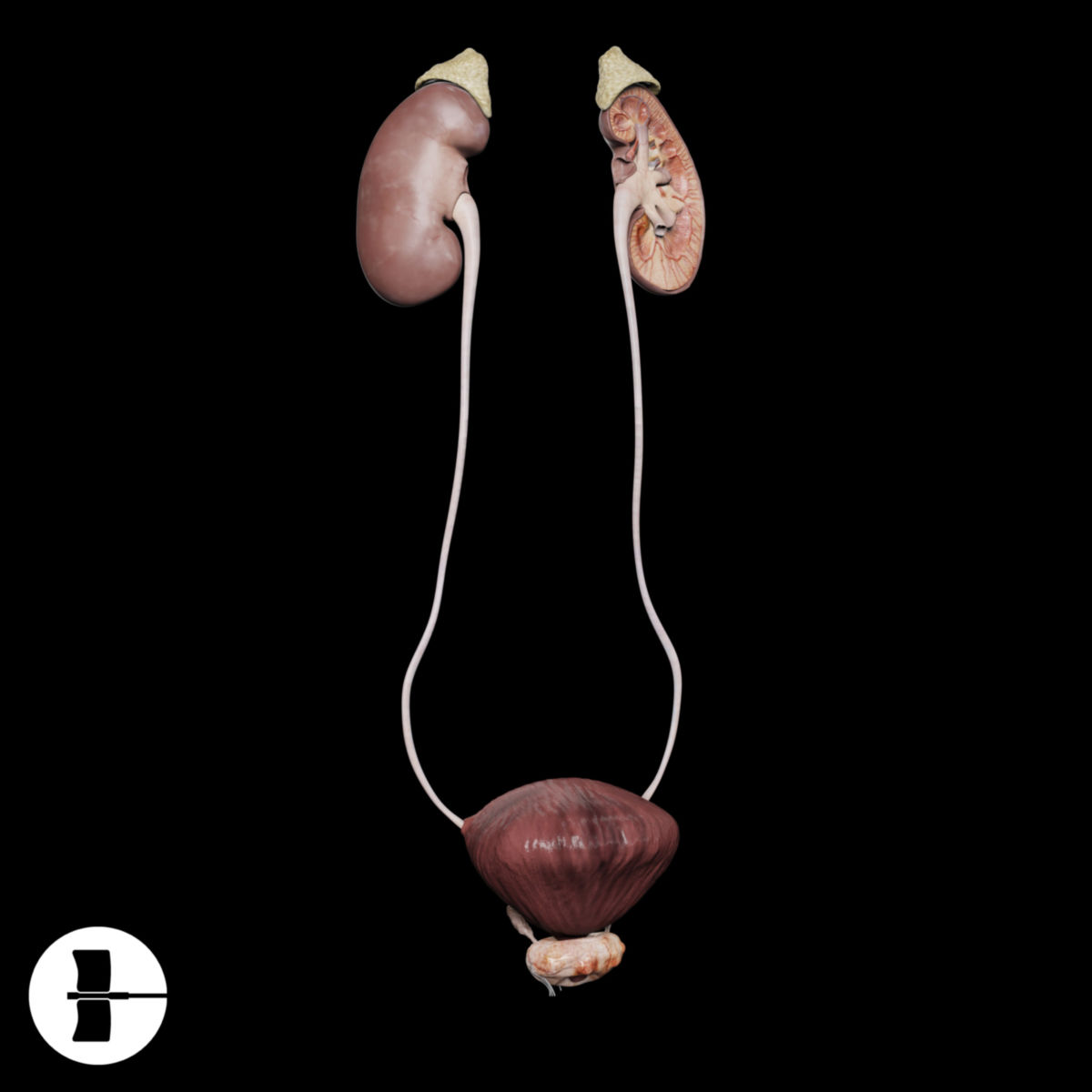
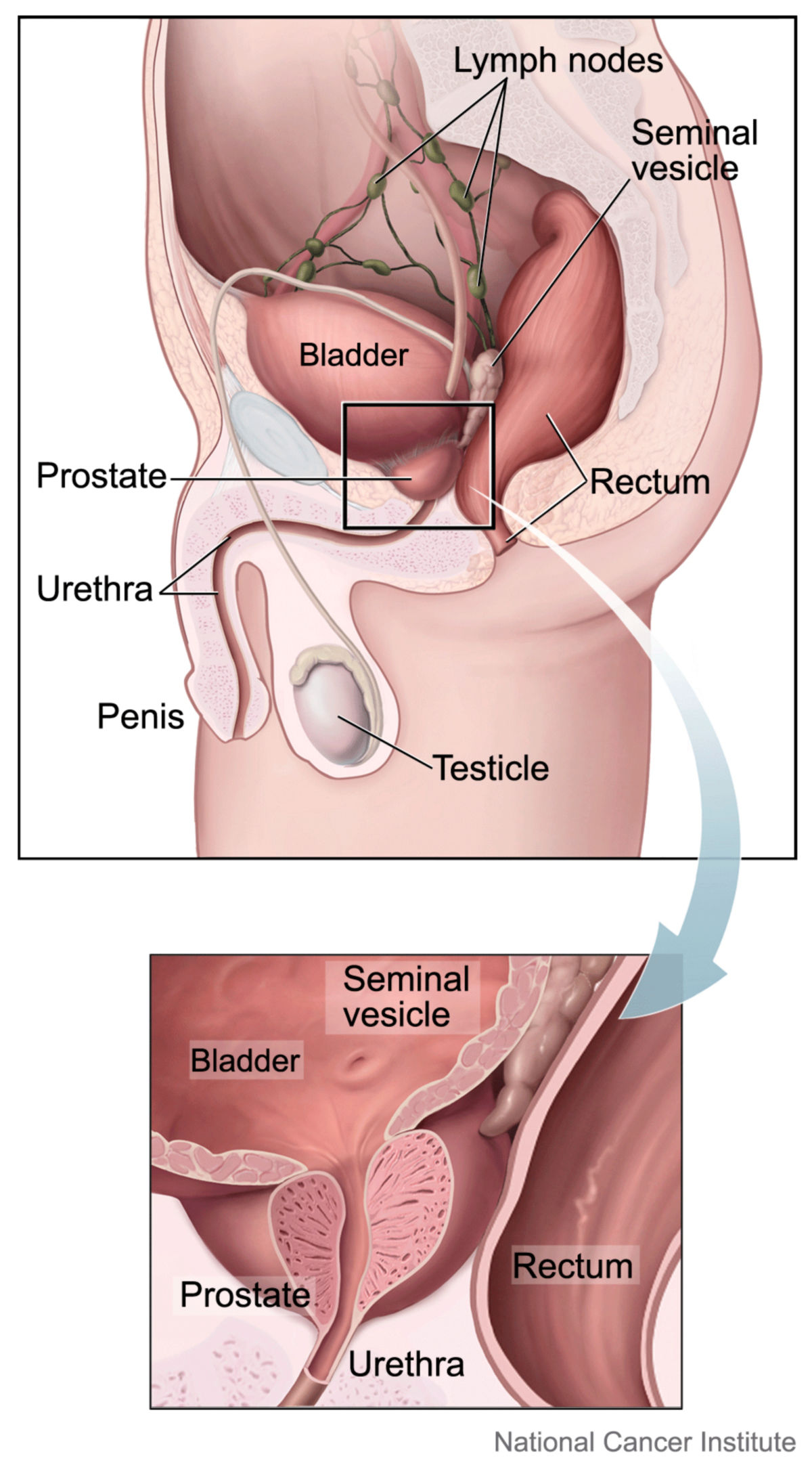
The prostate is an unpaired exocrine gland located below the urinary bladder, surrounding the male urethra. It is part of the accessory sex glands and contributes to seminal fluid by producing prostatic secretion.
In women, a corresponding structure is the paraurethral gland, also referred to as the female prostate.
2. Anatomy
2.1. Morphology
The prostate is located beneath the peritoneum, approximately the size of a chestnut, measuring 3 cm in length, 4 cm in width, and 2 cm in thickness. It weighs around 20 grams and has a firm, compact structure. Its shape is roughly pyramidal, with the base attached to the bladder's floor, while the tip points downward toward the urogenital diaphragm. The posterior surface is separated from the rectal ampulla by the rectoprostatic fascia, while the anterior surface is connected to the pubic symphysis via the puboprostatic ligament.
The second part of the urethra passes through the prostate, along with the ejaculatory ducts from the deferent duct, which join with the excretory duct of the seminal vesicles at the prostate's edge. The ejaculatory ducts open into the urethra at the seminal colliculus.
The prostate is surrounded by a thick, fibrous capsule. Its fibromuscular stroma consists of a connective tissue framework with abundant smooth muscle. Within the stroma, there are about 30-50 tubuloalveolar glands, whose excretory ducts open into the prostatic urethra near the seminal colliculus.
2.2. Anatomical classification
The prostate can be anatomically divided into three lobes and a connecting isthmus:
- Right lobe of the prostate
- Left lobe of the prostate
- Middle lobe of the prostate
- Prostatic isthmus
2.3. Vascular supply
The prostate receives its blood supply primarily from branches of the inferior vesical artery and the middle rectal artery, both of which originate from the internal iliac artery, providing blood flow dorsally and laterally. Ventrally, it is supplied by branches of the internal pudendal artery, and occasionally, the obturator artery may also contribute to its vascular supply.
Venous drainage occurs via the prostatic venous plexus, which drains into the vesical veins and ultimately into the internal iliac vein.
Lymphatic vessels from the prostate accompany the arteries, joining the ductus deferens. There are also connections to the lymph vessels of the bladder and rectum. The primary regional lymph nodes involved in prostate lymphatic drainage are the external iliac nodes, internal iliac nodes, and sacral lymph nodes.
2.4. Innervation
The autonomic innervation of the prostate is carried out by the prostatic plexus, which is an extension of the inferior hypogastric plexus. Sympathetic nerve fibers are responsible for stimulating the contraction of smooth muscle during ejaculation, facilitating the expulsion of prostatic secretions. Parasympathetic fibers, originating from spinal cord segments S3 and S4, travel through the pelvic splanchnic nerves to the inferior hypogastric plexus and promote glandular secretion.
Additionally, sensory fibers from the prostate project into the sacral spinal cord.[1] In rare cases, structures such as pacinian corpuscles may also be found within the prostate.[2]
3. Histology
3.1. Histopathological classification
In clinical practice, prostate tissue is often classified based on its histopathological characteristics rather than its anatomical structure. This functional categorization, commonly used in diagnostics and treatment, divides the prostate into different zones that are arranged concentrically around the urethra. The most widely accepted classification is based on studies by McNeal:
| Periurethral mantle zone | This zone constitutes of approximately 5 to 10 % of the prostate's total mass. It surrounds the urethra between the seminal colliculus and the bladder neck. |
| Transition zone | Comprising about 5 % of the prostate tissue, the transition zone consists of two paraurethral glandular lobes and is located on both sides of the periurethral mantle zone. |
| Inner zone | This zone makes up 20 to 25 % of the prostate mass and extends in a funnel shape from the bladder's cranial end to the seminal colliculus. It also includes the ejaculatory ducts. |
| Outer zone | Accounting for 70 % of the prostate's mass, the outer zone encloses the rest of the organ, particularly on its dorsolateral aspects. This zone is also the most common site for prostate cancers to develop. |
| Anterior zone | This narrow zone contains little to no glandular tissue and primarily consists of fibromuscular stroma. |
3.2. Glandular epithelium
The glandular epithelium of the prostate is a multi-layered epithelium, and its cells can appear tall, isoprismatic, or flat depending on secretory activity, hormonal influences, and age. These cells contain numerous secretory granules and vacuoles, which produce substances such as prostate-specific acid phosphatase. Additionally, the epithelial cells can release cytoplasmic droplets through apocrine secretion, and the correlates of this process are referred to as prostasomes in the ejaculate. The epithelial cells express markers like cytokeratin 8 and 18, as well as CD57.
3.3. Other cell types
Several other cell types are present in the prostate, including:
- Stromal cells: fibrocytes, smooth muscle cells
- Basal cells: progenitor cells located between the glandular cells and the basal membrane. They play a crucial role in renewing the glandular epithelium through proliferation. Basal cells express markers such as Bcl2, cytokeratin 5, and CD44.
- Mucin-producing cells
- Endocrine chromaffin cells: produce e.g. serotonin
3.4. Prostate stones
Histological sections of the prostate often reveal eosinophilic bodies, ranging from 0.2 to 2 mm in size, within the glandular lumina. These prostate stones are precipitates of prostatic secretions that have formed in layers, typically around exfoliated epithelial cells.
4. Embryology
The glandular epithelium of the prostate develops from the urogenital sinus at the level of the Wolffian duct opening and is derived from the endoderm. Starting around the 12th week of embryonic development, under the influence of androgens, specifically testosterone and dihydrotestosterone (DHT), the epithelial cells in this region begin to sprout into the surrounding mesenchyme, forming the glandular structure of the prostate. The mesenchyme differentiates into the stroma of the prostate. In female embryos, a similar process leads to the formation of the paraurethral gland.
The expression of the homeobox gene NKX3.1 is critical for the proper development of the prostate.
5. Secretion
Prostatic secretion constitutes 15 to 30 % of the total fluid in the ejaculate. It is thin and slightly acidic, with a pH of 6.4. The secretion contains numerous important components, including:
- Proteases (e.g. prostate-specific antigen): These enzymes help liquefy the seminal coagulum, enabling sperm to become motile.
- Zinc: Acts as a protease inhibitor, protecting sperm by forming a zinc-glycoprotein complex on the sperm membrane. It also plays a role in testosterone metabolism within the prostate.
- Citrate: Contributes to the buffering of seminal plasma
- Prostaglandins: Stimulate uterine contractions
- Spermine: Influences sperm motility and DNA stability. It also imparts the characteristic "chestnut blossom" odor to the secretion.
- Immunoglobulins
- Acid phosphatase
6. Physiology
Like other accessory sex glands, the prostate is highly responsive to hormones. After testosterone is taken up from the bloodstream, it is converted into dihydrotestosterone by the enzyme steroid 5α-reductase, particularly within stromal cells. This conversion triggers the release of growth factors, which in turn stimulate the proliferation of the glandular epithelium.
The prostate plays an important role in controlling urethral permeability. During erection or ejaculation, the prostate contracts to close off the urethra at the bladder outlet, preventing the mixing of urine with seminal fluid, which would otherwise negatively impact sperm function and fertilization.
Prostatic secretions are specifically formulated to liquefy sperm in the acidic environment of the vagina. This process counteracts the inhibitory effect of zinc on proteases, allowing the sperm to become more motile.
7. Clinic
7.1. Diagnostics
The prostate's outer zone, which makes up most of its mass, is located dorsally, making it accessible for diagnostic evaluation through digital rectal examination (DRE). This simple procedure can provide critical information about the presence of indurations or tenderness. For more detailed assessments, imaging techniques can be used, including:
- Transrectal ultrasound (TRUS)
- Multiparametric magnetic resonance imaging (MRI)
- Computed tomography (CT)
- Positron emission tomography (PET)
- Elastography
- Histo-scanning
If prostate cancer is suspected, biopsies are taken from suspicious areas, typically guided by imaging to increase diagnostic accuracy. The biopsy samples are then examined histologically to confirm the presence of malignancy.
7.2. Clinical pictures
Prostate diseases fall under the specialty of urology and include:
- Prostatitis
- Benign prostatic hyperplasia (BPH): usually in the transition zone or the periurethral zone
- Prostate carcinoma: Usually found in the peripheral (outer) zone of the prostate
Because the prostate is closely associated with parasympathetic nerves from the sacral cord, which control erection, erectile dysfunction is a frequent complication following prostate surgery.
7.3. Forensic medicine
In forensic investigations, spermine crystals from dried seminal fluid can be detected and used as evidence in legal cases.
8. Sources
9. Literature
- Schünke et al. Prometheus Lernatlas der Anatomie, 4th edition, Georg Thieme Verlag, 2015.