Corpus: Pituitary gland
Synonyms: hypophysis, glandula pituitaria
1. Definition
The pituitary gland is a hormone-producing organ in the central nervous system, about the size of a hazelnut. It synthesizes and releases a wide range of hormones and plays a central regulatory role in the body’s endocrine system.
2. Classification
- anterior pituitary (adenohypophysis): contains glandular cells whose activity is controlled by neurons of the hypothalamus, among others
- pars distalis
- pars tuberalis
- pars intermedia
- posterior pituitary (neurohypophysis): contains axon endings of hypothalamic neurons that produce effector hormones
- pars nervosa (lobus nervosus)
- pituitary stalk (infundibulum)
3. Embryology
3.1. Anterior pituitary
The anterior pituitary begins to develop in the 4th week of embryonic life. An ectodermal outgrowth (Rathke’s pouch) forms at the roof of the primitive mouth cavity, just in front of the buccopharyngeal membrane. It grows upward and attaches to the base of the brain (diencephalon). The connection to the mouth eventually disappears, but remnants can remain and may give rise to craniopharyngiomas.
As it matures, Rathke’s pouch expands to form the pars distalis and pars tuberalis. The back part becomes the smaller pars intermedia. The cavity of Rathke’s pouch normally disappears, though it may leave small colloid-filled cysts (pseudofollicles).
The development of the adenohypophysis depends on the coordinated action of specific transcription factors such as Prop-1, Pit-1, SF-1, T-Pit, and DAX-1. Mutations in these genes can lead to rare cases of selective or combined hormone deficiencies.
3.2. Posterior pituitary
Soon after Rathke’s pouch attaches to the base of the third ventricle, the neurohypophysis begins to form through thickening of the epithelium. This results in a downward bulge called the infundibular process, which becomes the pituitary stalk and the pars nervosa. From the third month on, epithelial cells start to differentiate into specific glial cells called pituicytes. Meanwhile, unmyelinated nerve fibers grow in from hypothalamic nuclei. A small cavity (infundibular recess) remains at the base of the infundibulum.
4. Anatomy
The pituitary gland weighs about 600 mg and measures approximately 13 x 9 x 6 mm. It is divided into an anterior lobe (pars distalis and pars intermedia) and a posterior lobe (pars nervosa). The approximately 3 mm long pituitary stalk connects the gland to the floor of the third ventricle.
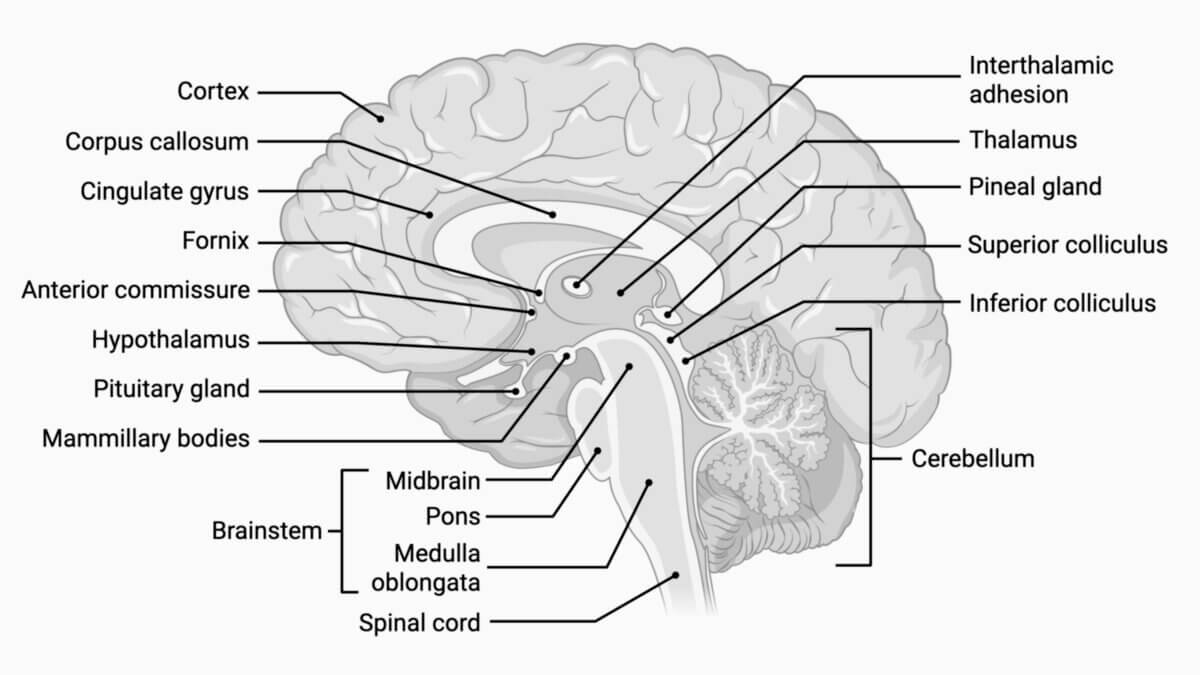
The pituitary sits at the base of the skull in a depression of the sphenoid bone called the sella turcica. A fold of dura mater (diaphragma sellae) covers it from above, with a small opening for the pituitary stalk.
Topographically, a distinction is made between a suprasellar (above the diaphragm) and an intrasellar part of the pituitary gland:
- Suprasellar part: includes the pituitary stalk and lies above the diaphragm, near the optic chiasm. Tumors here may cause loss of peripheral vision (bitemporal hemianopsia).
- Intrasellar part: includes the gland itself and lies within the sella turcica. It borders the cavernous sinus laterally, through which the internal carotid artery and several cranial nerves (the oculomotor nerve (CN III), trochlear nerve (CN IV), abducens nerve (CN VI), and branches of the trigeminal nerve (CN V) pass. The two cavernous sinuses are connected by venous channels, which play a role in procedures like inferior petrosal sinus sampling (IPSS).
4.1. Blood supply
The pituitary is supplied by two arteries on each side:
- Inferior hypophysial artery: arises from the internal carotid artery and supplies the posterior lobe
- Superior hypophysial artery: also branches from the internal carotid in the subarachnoid space and supplies the infundibulum and, indirectly, most of the anterior lobe. It connects with the inferior artery via its main branch, the trabecular artery.
The anterior lobe receives most of its blood through a portal vascular system. Branches of the superior hypophysial artery enter the infundibulum and form a capillary network. In the lower part of the infundibulum, anastomoses between the trabecular artery and the inferior hypophysial artery also form capillary loops. This area is known as the median eminence, which is part of the circumventricular organs — areas with capillaries that have a fenestrated endothelium and no blood-brain barrier.
Blood from this first capillary network drains into hypophysial portal veins, which transport it to the anterior lobe. There, the vessels form a second capillary network — sinusoidal capillaries — which are closely associated with the hormone-producing glandular cells. The blood from this second network is collected by small veins that empty into the cavernous sinus and intercavernous sinus.
This pituitary portal vascular system provides a direct and efficient link between the hypothalamus and the anterior pituitary. It allows even very small amounts of hypothalamic hormones to reach the anterior lobe rapidly and in high concentrations.
The pars nervosa of the posterior lobe is primarily supplied by the inferior hypophysial artery, along with some branches from the superior hypophysial artery. These vessels also form a dense capillary network with fenestrated endothelium, and like the median eminence, this area lacks a blood-brain barrier.
5. Histology
5.1. Anterior pituitary
The anterior pituitary is made up of epithelial cells arranged in clusters and cords. Between these cells lies collagen-rich connective tissue containing wide-lumen capillaries (sinusoids) lined by fenestrated endothelium.
Based on how their cytoplasm stains, the epithelial cells are classified as acidophilic, basophilic, or chromophobic cells. Immunohistochemical techniques allow further classification into hormone-producing cell types:
- Corticotropic cells: basophilic; produce derivatives of proopiomelanocortin (POMC), such as ACTH
- Thyrotropic cells: basophilic; produce thyroid-stimulating hormone (TSH)
- Gonadotropic cells: basophilic; produce follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
- Somatotropic cells: acidophilic; produce growth hormone (somatotropin or STH)
- Lactotropic cells: acidophilic; produce prolactin (PRL)
Between these hormone-producing cells are folliculostellate cells, which have long projections that connect with each other to form networks. They help regulate the activity of the epithelial cells by releasing signaling molecules.
Most hormone-producing cells are found in the pars distalis. The pars intermedia is only rudimentarily developed and mainly contains corticotropic cells that produce various POMC-derived hormones (e.g. α-MSH, β- and γ-lipotropin, β-endorphin). The exact functions of these hormones are still unclear (as of 2025).
The pars tuberalis is separated from the infundibulum of the neurohypophysis by a thin layer of connective tissue. Some of its cells produce FSH, LH, and TSH, but the role of most cells in this region remains unknown (as of 2025).
5.2. Posterior pituitary
More than 70 % of the posterior pituitary consists of unmyelinated axons whose cell bodies (perikarya) are located in the hypothalamus. These include axons from neurons that project to the anterior pituitary, as well as those from magnocellular neurons in the supraoptic and paraventricular nuclei, which extend into the posterior lobe. This system is known as the magnocellular neuroendocrine system.
The posterior pituitary also contains specialized glial cells called pituicytes, which make up about 25 % of the posterior lobe's volume. These cells are connected by highly branched projections and junctions.
The lobus nervosus also contains many sinusoidal capillaries with fenestrated endothelium. Like the median eminence, it is part of the circumventricular organs, meaning it lacks a blood-brain barrier.
Magnocellular neurons in the hypothalamus produce oxytocin and antidiuretic hormone (ADH). These hormones are synthesized as prohormones and cleaved to release the active hormone along with neurophysin I or II, which act as carrier proteins. The hormones are packed into secretory vesicles and transported down the axons to the posterior lobe. Large accumulations of these vesicles are known as Herring bodies. When these neurons are activated, the hormones are released (a process called neurosecretion) and enter the bloodstream through the fenestrated capillaries.
6. Physiology
6.1. Anterior pituitary
The anterior pituitary secretes various hormones in a pulsatile manner and is regulated by releasing and inhibiting hormones from the hypothalamus. These hypothalamic hormones are transported along the axons of hypothalamic neurons to the median eminence of the proximal infundibulum, where they are stored. In response to specific neural stimuli, these control hormones are released into the capillaries of the portal system and reach the anterior pituitary in high concentrations.
Functionally, a distinction is made between glandotropic hormones, which act on other endocrine glands, and non-glandotropic (effector) hormones, which act directly on target organs:
- Glandotropic hormones
- Thyroid-stimulating hormone (TSH)
- Adrenocorticotropic hormone (ACTH)
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH)
- Non-glandotropic hormones:
- Growth hormone (somatotropic hormone or STH)
- Prolactin
- Melanocyte-stimulating hormone (MSH)
6.2. Posterior pituitary
The posterior pituitary releases two hormones:
- Oxytocin: stimulates uterine contractions and induces labour; after birth, it causes milk ejection from the mammary glands by contracting myoepithelial cells; its role in men has not yet been clearly defined.
- Antidiuretic hormone (ADH): promotes water reabsorption in the distal tubules and collecting ducts of the kidney by increasing the number of aquaporin-2 channels in the apical membrane.
The activity of the magnocellular neuroendocrine neurons in the hypothalamus is regulated by both chemical signals (e.g. blood osmolarity) and nerve signals (e.g. inputs from the limbic system).
7. Diseases of the pituitary gland
- Hormone deficiency (hypopituitarism): Each hormone-producing part of the pituitary can fail individually or in combination. If the entire pituitary gland is affected, this is called panhypopituitarism (Simmond's syndrome).
- Hormone excess (hyperpituitarism): Any hormone-producing part of the pituitary can develop a benign tumour (pituitary adenoma) that leads to hormone overproduction. For example, increased secretion of growth hormone can lead to acromegaly.
8. Literature
- Benninghoff, Drenckhahn: Anatomie Band 2, 16. Auflage 2004, Elsevier: Urban & Fischer