Corpus: Dura mater
from Latin: durus - hard; mater - mother
Synonyms: meninges, dura
1. Definition
The dura mater is the outermost meninges (pachymeninx) that surrounds the central nervous system. It borders on the neighboring bones of the skull and spinal column.
2. Classification
The dura mater is classified based on its location:
- Cranial dura mater: surrounds the brain
- Spinal dura mater: surrounds the spinal cord
Both structures merge in the foramen magnum.
3. Anatomy
3.1. Overview
3.1.1. Cranial dura mater
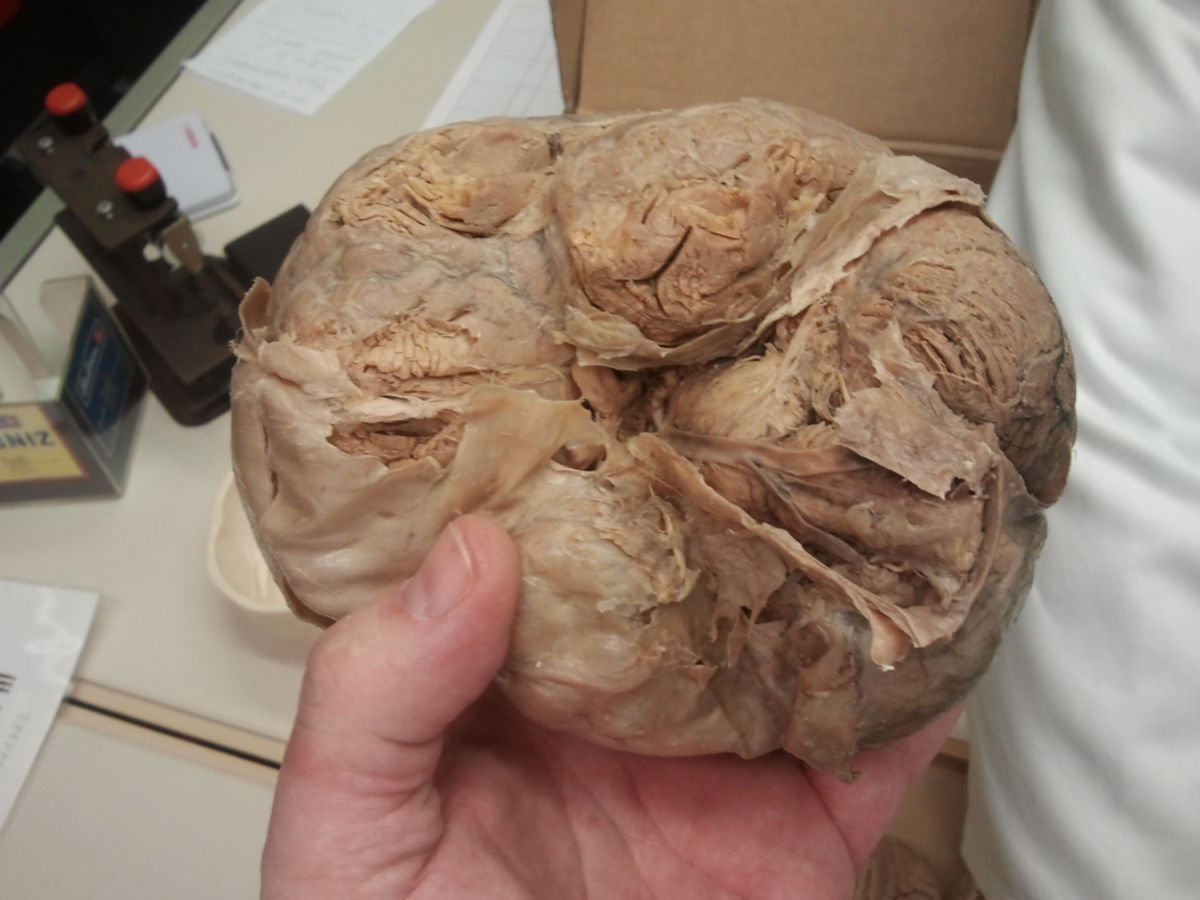
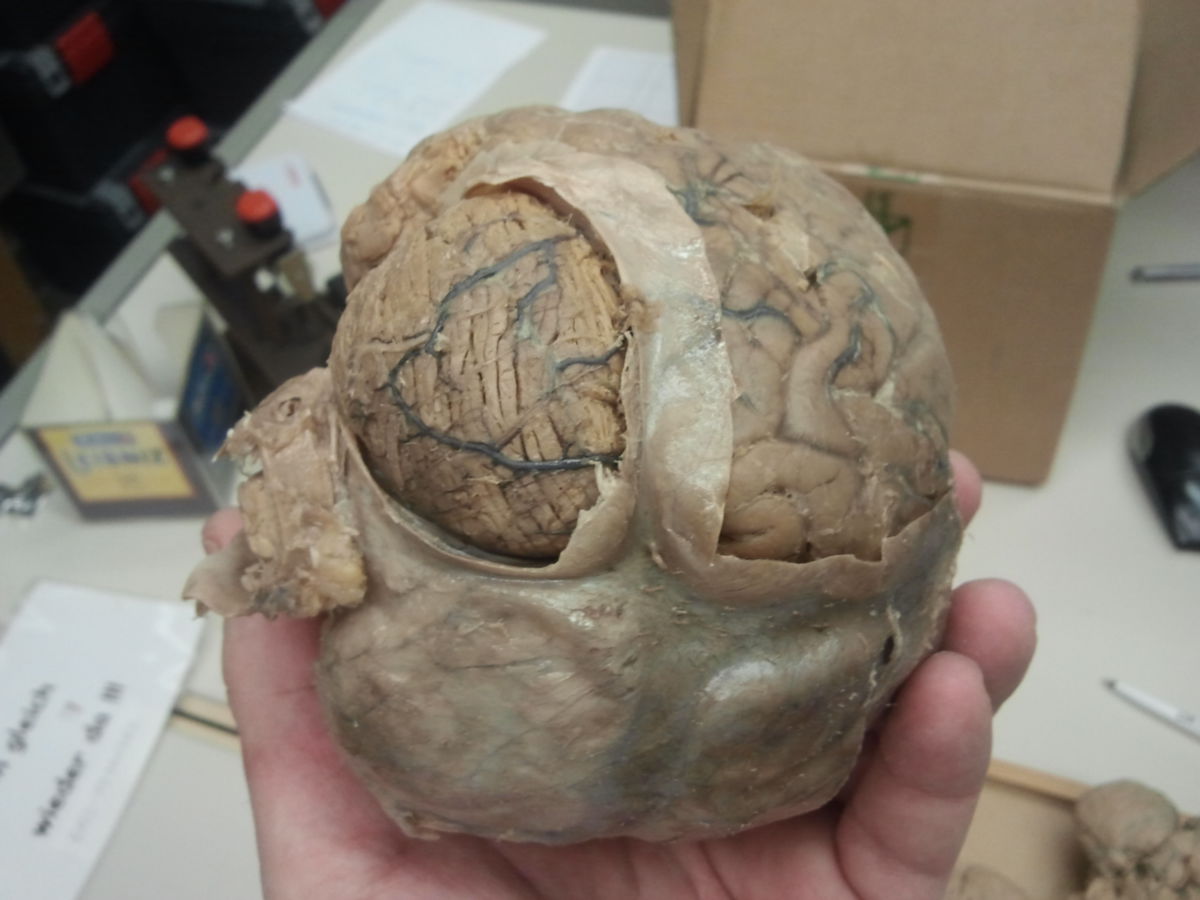
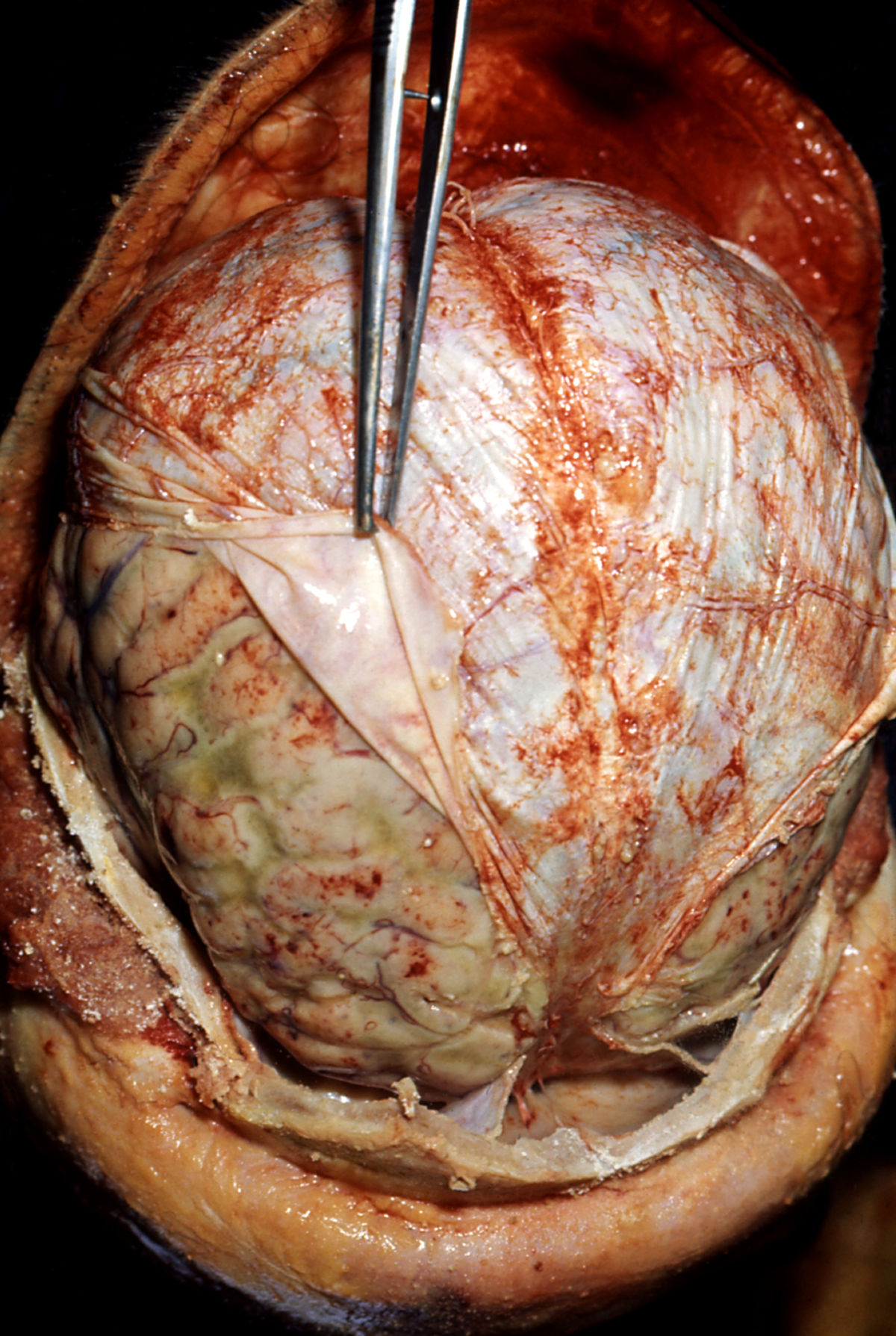
The cranial dura mater is located within the cranial cavity. It consists of two layers: an outer layer, known as the fibrous layer or periosteal layer, and an inner layer, known as the neurothelial layer or meningeal layer, which is adjacent to the arachnoid mater.
The fibrous layer is composed of dense connective tissue with numerous collagen and elastic fibers. Functionally, it acts as the periosteum of the cranial cavity, firmly attached to the cranial bones in many areas. At the foramina and sutures, it transitions seamlessly into the pericranium on the outer skull. In the orbital fissures, the dura mater continues into the periosteum of the orbital cavity (periorbita).
The inward-facing neurothelial layer is a multi-layered structure made up of epithelial-like meningeal cells (duraneurothelium). The tightly sealed, narrow intercellular gap between the innermost duraneurothelium and the outer arachnoid cell layer forms a diffusion barrier between the cerebrospinal fluid (CSF) and the blood vessels of the dura, part of the blood-CSF barrier. The duraneurothelium terminates at the exit points of the cranial nerves.
In some areas, the dura mater splits into two layers. The outer layer adheres to the skull bone, while the inner layer detaches and forms membranous structures that subdivide the cranial cavity into compartments:
- Falx cerebri in the longitudinal fissure between the cerebral hemispheres
- Tentorium cerebelli between the cerebrum and cerebellum
- Falx cerebelli between the cerebellar hemispheres
- cerebral dural covering of sinus of the dura mater and trigeminal cavity
- Diaphragma sellae
The falx cerebri and the tentorium cerebelli create a tension belt system that mechanically stabilizes the skull from within. The tentorium supports the pressure of the brain on the cerebellum and brainstem, while the falx and tentorium absorb mass shifts in the brain during trauma, reducing brain deformation.
3.1.2. Spinal dura mater
The spinal dura mater encases the spinal cord within the spinal canal, constituting an elongated dural sac. Like in the skull, the spinal dura consists of a fibrous layer and a neurothelial layer. However, the fibrous layer is not directly connected to the bone, as there is a separate periosteum. Thus, the dural sac is surrounded by an epidural space filled with loose connective tissue, numerous fat cells, and a venous plexus (internal vertebral venous plexus).
The dural sac is attached to the spinal canal wall and the posterior longitudinal ligament in certain areas. Lateral extensions (dural funnels) are formed for the spinal nerve roots' exits. At the intervertebral foramina, the dura transitions seamlessly into the connective tissue capsule and the epineurium of the spinal ganglia and nerves.
The dural sac narrows in the mid-thoracic region and widens in the cervical and lumbar regions (cisterna lumbalis). In the sacral canal, it tapers conically and merges into the dural part of the filum terminale.
In some texts, the periosteum of the vertebral bodies is referred to as the outer layer of the dura mater (endorhachis), while the dural sac is formed by the inner layer (meningeal layer). Thus, the epidural space lies between the inner and outer dura layers.
3.2. Blood vessels
3.2.1. Cranial dura mater
The cranial dura mater includes the sinus durae matris, which collects venous blood from the brain and directs it to the internal jugular veins on both sides.
The meningeal vessels form the private blood supply of the cranial dura mater, including:
- Anterior meningeal artery of the anterior ethmoidal artery
- Meningeal branch of the posterior ethmoidal artery
- Middle meningeal artery of the maxillary artery
- Meningeal branch from the internal carotid artery
- Posterior meningeal artery of the ascending pharyngeal artery
- Meningeal branch of the vertebral artery
- Meningeal branch of the occipital artery
The meningeal veins, such as the middle meningeal veins, usually accompany the arteries and sometimes drain directly into the sinus durae matris.
3.2.2. Spinal dura mater
The spinal dura mater has a well-developed capillary network with partially fenestrated endothelium. This system is supplied by dural branches and radicular arteries from various spinal branches, connected ventrally and dorsally to the vertebral artery. In the upper cervical region, there are direct connections to the meningeal arteries of the vertebral and posterior cerebellar arteries. Blood drains through the venous plexus and radicular veins.
3.3. Lymphatic vessels
The dura has lymphatic capillaries and collectors near nerve root exits, primarily accompanying the meningeal veins. The dura mater spinalis contains lymphatic capillaries at the spinal cord nerve exit points.
3.4. Innervation
3.4.1. Cranial dura mater
The cranial dura mater is highly sensitive to pain, with sensory innervation provided by the meningeal branches of the following nerves:
- Glossopharyngeal nerve
- Vagus nerve
- Mandibular nerve (V3)
- Maxillary nerve (V2)
- Ophthalmic nerve (V1)
- Cervical spinal nerves (C1-3)
Parasympathetic fibers originate from the ciliary, pterygopalatine, and otic ganglia, as well as scattered ganglion cell groups near the superior sagittal sinus. Sympathetic fibers arise from the superior cervical ganglion, entering the dura mater mainly via periarterial plexuses with the meningeal arteries and internal carotid artery.
3.4.2. Spinal dura mater
The spinal dura mater receives sensory supply from the meningeal branches of the spinal nerves. These fibers travel back through the intervertebral foramina to the dura. Noradrenergic efferents originate from the sympathetic border ganglia and reach the dura mater via periarterial plexuses.
4. Embryology
The dura mater develops from the outer layer of a mesenchymal condensation called the primitive meninx. This ectomeninx forms around the sixth embryonic week.
5. Clinic
The high proportion of peptidergic axons (CGRP, substance P) in the meninges is linked to certain headaches, such as migraines.
During space-occupying processes, the dura folds cannot entirely prevent brain displacement and entrapment. For example, parts of the temporal lobe can become trapped in the tentorial slit, compressing the oculomotor nerve (upper entrapment). Parts of the cerebellum can be pushed into the foramen magnum by brain pressure (lower entrapment).
During a craniotomy, the fibrous layer of the dura must be separated from the skull bone. If not done properly, the dura detaches from the arachnoid, forming an artificial subdural space, which can also result from hemorrhage, such as after a bridging vein rupture.
Bleeding from the meningeal arteries can detach the dura from the bone, leading to an epidural hematoma. This can also occasionally arise from ruptured meningeal veins.
Idiopathic hypertrophic pachymeningitis (IHP) is a rare disease that causes dura mater thickening, classified as an IgG4-associated disease.[1]
By puncturing the epidural space in the spinal canal and administering a local anesthetic, nerve anesthesia can be achieved (epidural anesthesia). In contrast, spinal anesthesia involves administering the anesthetic in the subarachnoid space.
6. Literature
- Nimer Adeeb, Martin M Mortazavi, R Shane Tubbs, Aaron A Cohen-Gadol: The cranial dura mater: a review of its history, embryology, and anatomy Childs Nerv Syst. 2012 Jun;28(6):827-37. doi: 10.1007/s00381-012-1744-6. Epub 2012 Apr 15. PMID: 22526439
7. Source
- ↑ de Girgilio A et al. Idiopathic hypertrophic pachymeningitis: an autoimmune IgG4-related disease, Immunol Res. 2017;65(1):386-394, accessed 15 July 2020