Corpus: Ureter
from ancient Greek: ourein - to let water, urinate
1. Definition
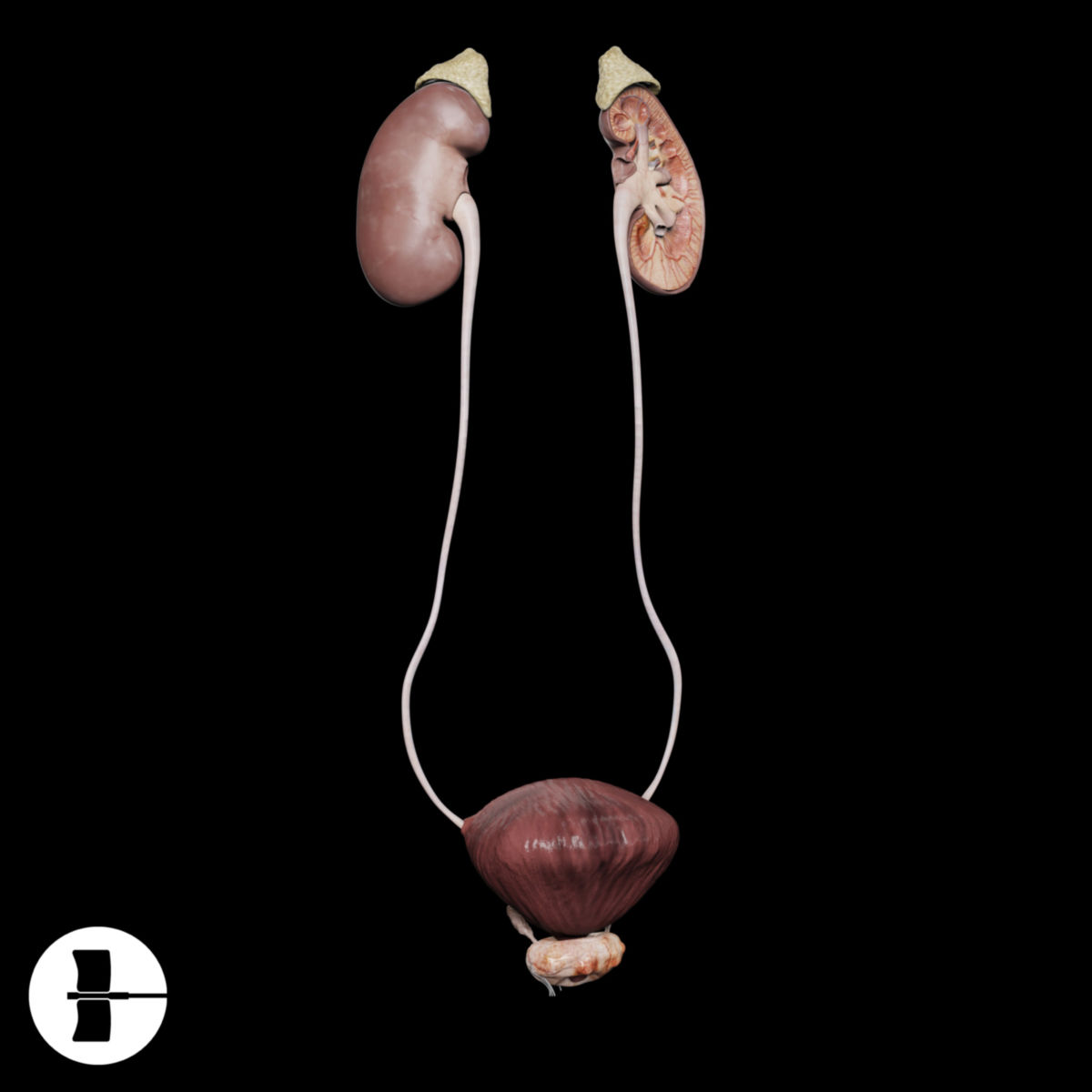
The ureters are paired, muscular, hollow organs within the urogenital system responsible for transporting urine from the renal pelvis to the urinary bladder. It's important to note that using the Latin term "ureter" can sometimes lead to confusion with the term "urethra."
2. Anatomy
The ureters are approximately 25 to 30 cm in length and have a diameter of 4 to 7 mm. They originate in the renal pelvis, exit the kidney through the hilum, and terminate in the urinary bladder. The ureters are divided into three sections:
- Abdominal part: This section runs along the posterior abdominal wall from the kidney to the linea terminalis.
- Pelvic part: This section extends from the pelvic brim (linea terminalis) to the urinary bladder.
- Intramural part: This short segments passes obliquely through the bladder wall, where muscles actively close it at the bladder's entrance, playing a crucial role during urination by preventing backflow.
2.1. Course
The ureters travel through the retroperitoneal space, descending from the kidney along the medial edge of the psoas major muscle to the urinary bladder in the lesser pelvis.
As they pass over the psoas major muscle, the ureters initially cross over the genitofemoral nerve. In men, the ureters then pass under the ipsilateral testicular artery and vein, while in women, they pass under the ovarian artery and vein. Next, the ureters cross over the common iliac artery and vein. The external iliac veins is crossed less frequently. Near the sigmoid colon, the left ureter passes beneath the intersigmoid recess.
Further down, in women, the ureters pass beneath the uterine artery within the broad ligament (ligamentum latum). In men, they pass beneath the deferent duct in men, before entering the urinary bladder at the two ureteral orifices, which are located approximately 4 cm apart. At this point, they traverse the bladder wall at an angle, forming a valve system known, which prevents urine backflow into the kidneys (vesicorenal reflux).
The ureters are visible within the bladder mucosa as converging ridges (columnae uretericae), which extend downward as a fine transverse fold (plica ureterica), defining the boundaries of the bladder's trigone (trigonum vesicae).
2.1.1. Crossings
The course of the ureters can be remembered using the "over-under-over-under rule":
- Over the genitofemoral nerve
- Under the testicular or ovarian vessels
- Over the common iliac vessels
- Under the deferent duct in men and the uterine artery in women
2.2. Ureteral strictures
There are three physiological constrictions along the ureter:
- Upper ureteral stricture: At the transition from the renal pelvis to the ureter.
- Middle ureteral stricture: Where the ureter crosses the common or external iliac artery.
- Lower ureteral stricture: Where the ureter passes through the bladder wall.
Occasionally, the point where the ureter passes under the testicular or ovarian vessels acts as an additional constriction.
2.3. Blood vessels
The ureter is supplied by small branches from nearby large arteries.
2.3.1. Arterial supply
The ureter is supplied by arteries from rami ureterici, which originate from the arteries in its neighbourhood:
- Abdominal part: Supplied by branches from the renal artery and the testicular (in men) or ovarian artery (in women).
- Pelvic part: Supplied by branches from the common iliac artery, external iliac artery, and internal iliac artery, including visceral branches such as the uterine artery or artery of the deferent duct, and the inferior vesical artery.
2.3.2. Venous outflow
The veins follow the arteries and are named accordingly.
2.4. Innervation
The ureter receives sympathetic innervation via the aorticorenal ganglia and the inferior hypogastric plexus. Parasympathetic innervation is provided by the pelvic splanchnic nerves (from spinal segments S2-S4) and partly by the vagus nerve. Sympathetic stimulation inhibits ureteral peristalsis, while parasympathetic stimulation promotes it.
3. Histology
The lumen of the ureters is lined with transitional epithelium (urothelium), which rests on a thin layer of connective tissue. The adjacent longitudinal and circular muscle layers facilitate peristalsis. Externally, the ureters are enveloped by connective tissue and are covered with a mesothelial layer facing the peritoneum. Histologically, three layers can be distinguished from the inside (near the lumen) to the outside:
3.1. Mucosa
The innermost layer, which forms longitudinal folds that create a star-shaped lumen when the ureter is empty. It is composed of urothelium (transitional epithelium) that rests on a thin layer of connective tissue (lamina propria). The urothelium is covered apically by a protective layer called the crusta, which shields the cells from urine. The tunica mucosa lacks both a lamina muscularis mucosae and a submucosa layer.
3.2. Muscular layer
This middle layer consists of two to three layers of smooth muscle. In the abdominal part of the ureter, the tunica muscularis has two layers: an inner longitudinal layer and an outer circular layer. In the pelvic part, a third outer longitudinal layer, also known as the Waldeyer sheath, is added. This layer transitions into the trigonal muscle of the bladder. The muscle layers are interwoven with connective tissue, forming a functional unit that facilitates peristalsis.
3.3. Adventitia
The adventitia is the outermost layer, composed primarily of loose connective tissue containing blood and lymphatic vessels, as well as nerve fibers.
4. Physiology
The ureters do not transport urine continuously from the renal pelvis to the urinary bladder; instead, they use wave-like movements of the smooth muscles, known as ureteral peristalsis. These periodic contractions begin at the renal pelvis and occur approximately every 20 to 25 seconds. Thus, the ureter is not a passive, open "drainage pipe," but rather an active structure that collects urine in small portions by relaxing its wall muscles. The urine is then actively transported downward by subsequent muscle contractions, even against the force of gravity if necessary.
5. Clinic
Urinary stones, which form in the renal calices or renal pelvis, are a clinically significant condition. These stones often become lodged in one of the natural constrictions of the ureter and are therefore referred to as ureteral stones. The ureter attempts to expel the stone by actively contracting its walls, which results in severe pain known as "renal colic." However, the more accurate term for this condition is ureteral colic. The diagnosis can be confirmed by X-ray and computed tomography (CT). Therapeutic options for ureteral stones include "flushing out" the stones or removing them using extracorporeal shock wave lithotripsy (ESWL). Surgical intervention, such as ureterolithotomy, is only required for stones that cannot be removed by other means.
Urothelial carcinomas can also develop in the ureter, although these are rare.
Ectopic ureters, which do not open into the trigonum vesicae — as seen in cases of a double kidney with a duplicated ureter — typically lack an intramural section and are thus not protected against urine reflux. This condition can present as kidney pain during urination due to the transmission of intravesical pressure to the affected kidney. Over time, it may lead to recurrent renal pelvic inflammatory disease.
6. Sources
- Ulfig N: Short textbook histology. 4th, corrected edition. Thieme-Verlag