Corpus: Coronary artery: Unterschied zwischen den Versionen
(Bis Abschnitt "Overview" übersetzt) |
Keine Bearbeitungszusammenfassung |
||
| Zeile 1: | Zeile 1: | ||
''from Latin: corona - wreath, crown '' | ''from Latin: corona - wreath, crown '' | ||
| Zeile 38: | Zeile 36: | ||
** Right marginal branch | ** Right marginal branch | ||
** Posterolateral branch of the right ventricle (RPLD) | ** Posterolateral branch of the right ventricle (RPLD) | ||
** Atrioventricular node branch | ** [[Corpus:Atrioventricular node|Atrioventricular node]] branch | ||
** Posterior interventricular branch (RPD, right posterior descending artery) | ** Posterior interventricular branch (RPD, right posterior descending artery) | ||
** Septal branches (posterior septal branches) | ** Septal branches (posterior septal branches) | ||
| Zeile 45: | Zeile 43: | ||
===Arteria coronaria sinistra=== | ===Arteria coronaria sinistra=== | ||
The left coronary artery (LCA) originates from the left aortic sinus, just behind the attachment of the [[Corpus:Aortic valve|aortic valve]]. In about 75 % of cases, it is more prominent than the right coronary artery. It travels a short distance between the conus arteriosus and the aorta before dividing into two main branches: the Left Anterior Descending artery (LAD, also known as the anterior interventricular artery) and the Circumflex artery (LCx). | |||
In Bland-White-Garland syndrome, the LCA abnormally arises from the left [[Corpus:Pulmonary artery|pulmonary artery]] rather than the aortic sinus. | |||
==== Left Anterior Descending Artery (LAD) ==== | |||
The LAD runs downward in the anterior interventricular groove, wraps around the heart's apex, and anastomoses with the posterior interventricular branch of the right coronary artery in the posterior interventricular groove. The LAD gives off the following branches: | |||
* Conus artery: supplies the conus arteriosus. | |||
* Diagonal branch (ramus anterolateralis, ramus diagonalis, RD): supplies the anterior wall of the left ventricle (subject to anatomical variation). | |||
* Septal branches (rami septales anteriores): penetrate the [[Corpus:Interventricular septum|interventricular septum]] and supply it via superior, inferior, and apical septal branches. A mid-septal branch may also arise, which supplies the anterior [[Corpus:Papillary muscle|papillary muscle]] of the right ventricle via the moderator band. | |||
* | |||
* | |||
====Ramus circumflexus==== | ====Ramus circumflexus==== | ||
The circumflex | The circumflex artery follows the coronary groove on the left side, running posteriorly toward the diaphragmatic surface of the heart. Its branches include: | ||
* | |||
* Sinoatrial nodal branch: supplies the [[Corpus:Sinus node|sinus node]]; present in one-third of cases and may arise from either the LCx or right coronary artery. | |||
* Atrioventricular branches: these divide into atrial and ventricular branches, supplying the left atrium and left ventricle. | |||
* | * Left marginal branch: runs down along the obtuse margin of the left ventricle. | ||
* | * Intermediate atrial branch: supplies the posterior aspect of the left atrium. | ||
* Atrial anastomotic branch: small branch that forms an anastomosis with branches of the right coronary artery, sometimes supplying the atrioventricular node. | |||
* | * Posterolateral branch of the left ventricle: supplies the diaphragmatic surface of the left ventricle. | ||
* | |||
* | ==== Supply Areas ==== | ||
The areas supplied by the left coronary artery include: | |||
* The anterior wall of the left ventricle (via the LAD and diagonal branches). | |||
The | * Part of the anterior wall of the right ventricle (via the conus artery and LAD). | ||
* The anterior two-thirds of the interventricular septum (via the septal branches). | |||
* | * The left atrium (via atrial branches). | ||
* anterior two thirds of the | * The lateral and posterior walls of the left ventricle, except for the area near the posterior interventricular groove. | ||
* left atrium ( | |||
* left ventricle | |||
===Arteria coronaria dextra=== | ===Arteria coronaria dextra=== | ||
The right coronary artery (RCA) arises from the ascending aorta, specifically from the right aortic sinus, located just behind the aortic valve. It travels between the conus arteriosus and the right atrial appendage to reach the right side of the coronary groove (sulcus). From there, it continues along the groove to the diaphragmatic surface of the heart. At the crux of the heart (the point where the coronary sulcus and the interventricular sulcus meet), it gives off its final branch, the posterior descending artery (PDA, also called the posterior interventricular artery), which runs in the posterior interventricular groove toward the apex and connects with the anterior interventricular artery (LAD) from the left coronary artery. | |||
====Branches==== | |||
The RCA gives off the following branches: | |||
* Conus artery: supplies the conus arteriosus and part of the anterior wall of the right ventricle. | |||
* Sinoatrial nodal branch: runs along the front part of the right atrium and usually reaches the sinoatrial node via the terminal groove (sulcus terminalis). | |||
* Atrioventricular branches: these supply the anterior sections of the right atrium and ventricle. | |||
* Atrial branches: supply the lateral parts of the right atrium. | |||
* Right marginal branch: runs along the acute margin (margo acutus) of the right ventricle. | |||
* Posterolateral right ventricular branch: runs parallel to the right marginal branch along the posterior aspect of the right ventricle. | |||
* Atrioventricular nodal branch: arises just before the posterior descending artery and runs through the epicardial fat beneath the atrial septum to supply the atrioventricular (AV) node. | |||
* Posterior descending artery (PDA): the terminal branch of the RCA, which anastomoses with the anterior interventricular artery (LAD) from the left coronary artery. | |||
* Interventricular septal branches: these branches supply the ventricular septum, including the [[Corpus:Bundle of His|bundle of His]] and parts of the conduction system. | |||
** Anterior superior septal branches: arise directly from the RCA to supply the upper part of the septum. | |||
** Posterior superior and inferior septal branches: branch off from the posterior descending artery. | |||
==== | ====Supply area==== | ||
The | The right coronary artery supplies the following structures: | ||
* Sinoatrial node (via the sinoatrial nodal branch). | |||
* Atrioventricular node (via the atrioventricular nodal branch). | |||
* | * Right atrium (via atrial branches). | ||
* | * Part of the posterior wall of the left ventricle (via the posterolateral right ventricular branch). | ||
* Right atrium ( | * Right ventricle: | ||
* | ** Anterior wall (via conus artery and right marginal branch). | ||
* Right ventricle: Anterior wall ( | ** Lateral wall (via right marginal branch). | ||
* Ventricular septum | ** Posterior wall (via the posterior descending artery). | ||
* Ventricular septum: the smaller, posterior portion, including the conduction system (e.g., bundle of His) (via septal branches). | |||
==Abbreviations== | ==Abbreviations== | ||
| Zeile 110: | Zeile 109: | ||
! width=25% align="left" | '''English'''' - short || width=25% align="left" | '''Latin''' - short || width=50% align="left" | '''Long names'''' | ! width=25% align="left" | '''English'''' - short || width=25% align="left" | '''Latin''' - short || width=50% align="left" | '''Long names'''' | ||
|- | |- | ||
| valign="top" | RCA || valign="top" | ACD || valign="top" | '''r | | valign="top" | RCA || valign="top" | ACD || valign="top" | '''r'''ight '''c'''oronary '''a'''rtery<BR>'''A'''rteria '''c'''oronaria '''d'''extra | ||
|- | |- | ||
| valign="top" | LCA, LMCA || valign="top" | ACS || valign="top" | '''l'''eft '''c'''oronary '''a'''rtery<BR>'''l'''eft '''m''''ain '''c'''oronary '''a'''rtery<BR>'''A'''rteria '''c'''oronaria '''s'''inistra | | valign="top" | LCA, LMCA || valign="top" | ACS || valign="top" | '''l'''eft '''c'''oronary '''a'''rtery<BR>'''l'''eft '''m''''ain '''c'''oronary '''a'''rtery<BR>'''A'''rteria '''c'''oronaria '''s'''inistra | ||
| Zeile 116: | Zeile 115: | ||
| valign="top" | LAD || valign="top" | RIVA || valign="top" | '''l'''eft '''a'''nterior '''d'''escending coronary artery<BR>'''R'''amus '''i'''nter'''v'''entricularis '''a'''nterior | | valign="top" | LAD || valign="top" | RIVA || valign="top" | '''l'''eft '''a'''nterior '''d'''escending coronary artery<BR>'''R'''amus '''i'''nter'''v'''entricularis '''a'''nterior | ||
|- | |- | ||
| td valign="top" | LCx || valign="top" | RCX || valign="top" | '''l | | td valign="top" | LCx || valign="top" | RCX || valign="top" | '''l'''eft '''c'''ircumfle'''x''' coronary artery<BR>'''R'''amus '''c'''ircumfle'''x'''us | ||
|- | |- | ||
| valign="top" | RPD, R-PDA || valign="top" | RIVP || valign="top" | '''r'''ight '''p | | valign="top" | RPD, R-PDA || valign="top" | RIVP || valign="top" | '''r'''ight '''p'''osterior '''d'''escending coronary artery<BR>'''R'''amus '''i'''nter'''v'''entricularis '''p'''osterior | ||
|- | |- | ||
| valign="top" | RPLA || valign="top" | RPLD || valign="top" | '''r'''ight '''p'''ostero'''l'''ateral '''a'''rtery <BR>'''R'''amus '''p'''ostero'''l'''ateralis '''d'''exter | | valign="top" | RPLA || valign="top" | RPLD || valign="top" | '''r'''ight '''p'''ostero'''l'''ateral '''a'''rtery <BR>'''R'''amus '''p'''ostero'''l'''ateralis '''d'''exter | ||
| Zeile 125: | Zeile 124: | ||
==Supply types== | ==Supply types== | ||
The exact | The exact areas supplied by the coronary arteries and their branches can vary significantly between individuals. For instance, in about 20 % of cases, the posterior descending artery (PDA) originates from the left coronary artery (LCA), and in 10 % of cases, it arises from both the right and left coronary arteries (codominant supply type). | ||
In | In roughly 55 % of cases, the heart has a balanced supply type (normal supply type), where the posterior wall of the heart receives blood supply approximately equally from both the right and left coronary arteries. | ||
In 15 to 20 % of cases, the | In 15 to 20 % of cases, the left coronary artery is more dominant (left supply type). In this situation, the circumflex branch (LCx) extends to form the posterior descending artery, which supplies not only the posterior wall of the heart but also a part of the right ventricle and the posterior portion of the interventricular septum. | ||
In the right supply type (15 to 25 % of cases), the right coronary artery and | In the right-dominant supply type (occurring in 15 to 25 % of cases), the right coronary artery (RCA) and particularly its posterolateral branch are more developed. This branch supplies most of the posterior wall of the heart as well as the interventricular septum. | ||
== Anatomical variants== | == Anatomical variants== | ||
===Trifurcation=== | ===Trifurcation=== | ||
In some individuals, an additional artery arises from the point where the left main coronary artery divides into the LAD (left anterior descending) and the circumflex (LCx). This creates a trifurcation, where a third branch, called the intermediate artery (ramus intermedius), runs along the free wall of the left ventricle toward the apex. This variant is found in about 20 % of the population. | |||
===Single coronary artery=== | ===Single coronary artery=== | ||
A single coronary artery (SCA) is a rare congenital anomaly. The Lipton classification | A single coronary artery (SCA) is a rare congenital anomaly in which only one coronary artery arises from the aorta to supply the heart. The Lipton classification is used to categorize the different subtypes of this anomaly into three main groups:<ref>Lipton et al, Isolated Single Coronary Artery: Diagnosis, Angiographic Classification, and Clinical Significance. Radiology, 1979.</ref><ref>Katekaru-Tokeshi et al, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8397023/ Applicability of the Leiden Convention and the Lipton Classification in Patients with a Single Coronary Artery in the Setting of Congenital Heart Disease]. Journal of Cardiovascular Development and Disease, 2021</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
!group | !group | ||
| Zeile 149: | Zeile 148: | ||
|- | |- | ||
|IIA | |IIA | ||
|Anterior | |Anterior to the pulmonary trunk | ||
|RIIA / LIIA | |RIIA / LIIA | ||
|- | |- | ||
| Zeile 170: | Zeile 169: | ||
==Physiology== | ==Physiology== | ||
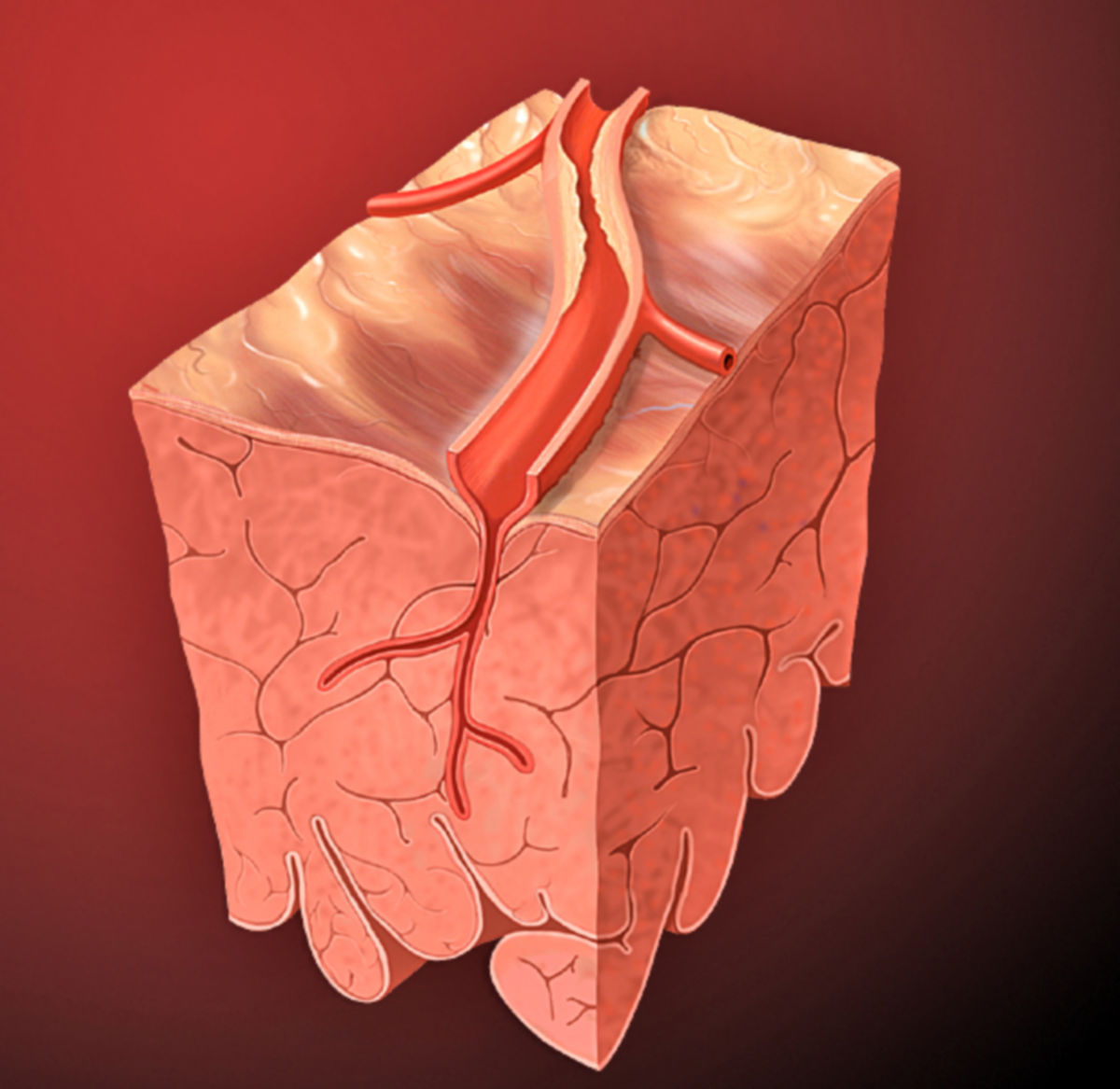
The heart relies on a constant supply of oxygen due to its high workload, making the function of the coronary arteries essential for the heart muscle. The coronary arteries form numerous connections ([[Corpus:Anastomosis|anastomoses]]) with each other, but these are not sufficient to create a fully redundant collateral circulation (referred to as "functional end arteries"). If one of the coronary branches becomes blocked, it leads to ischemia (lack of blood supply) in the affected area, followed by necrosis (tissue death) of the heart muscle. During increased cardiac activity, vasodilation (widening) of the coronary vessels is primarily mediated by metabolic by-products, such as carbon dioxide (CO), released by the endothelium. | |||
== | ==Clinical significance== | ||
===Diseases=== | ===Diseases=== | ||
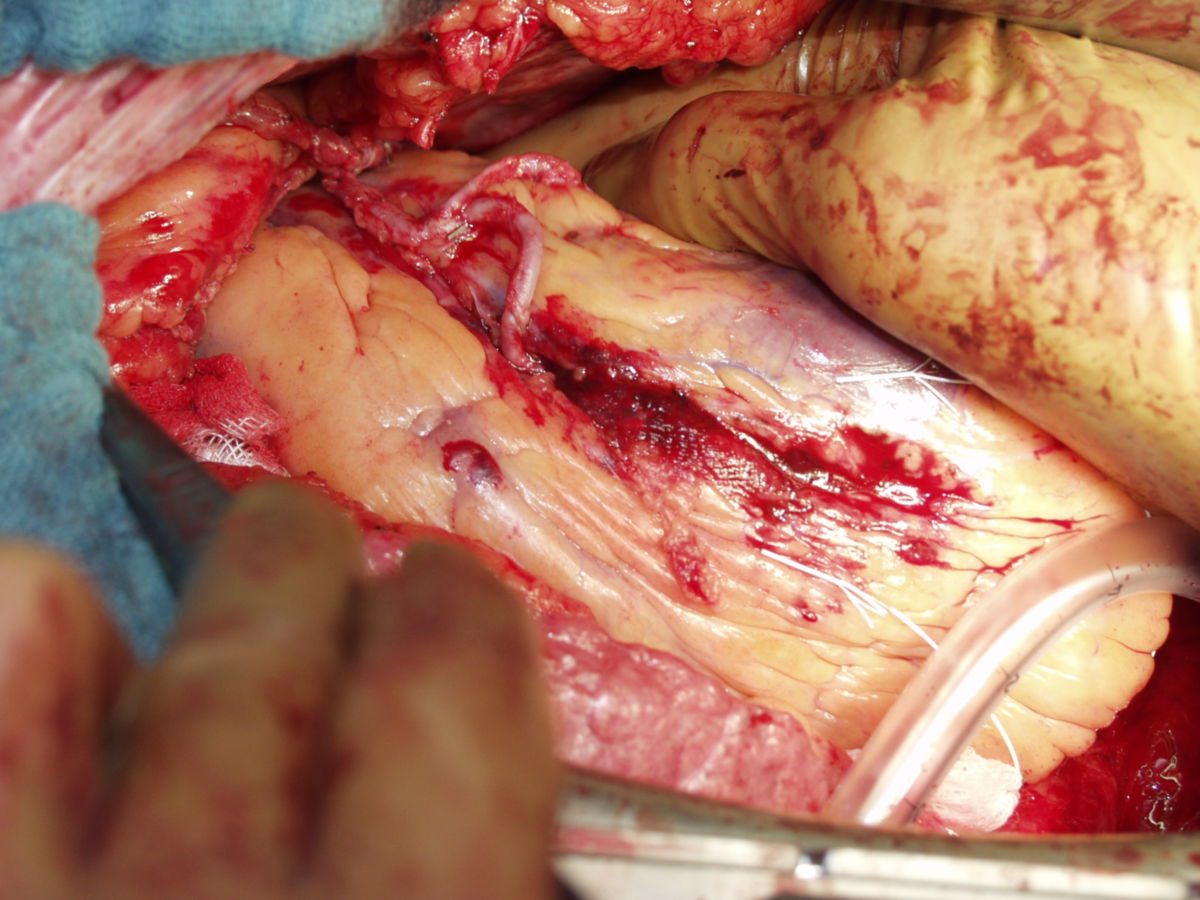
The most | The most significant disease affecting the coronary arteries is atherosclerosis, which causes narrowing (stenosis) or gradual blockage of the coronary arteries. This condition is known as coronary artery disease (CAD) or coronary heart disease (CHD). Clinically, it manifests as chest pain (angina pectoris), heart attack (myocardial infarction), or heart failure. CHD can be categorized based on the number of coronary vessels affected: | ||
*Single vessel disease | |||
*Two-vessel disease | * Single-vessel disease | ||
* | * Two-vessel disease | ||
*main | * Three-vessel disease | ||
* Left main coronary artery stenosis | |||
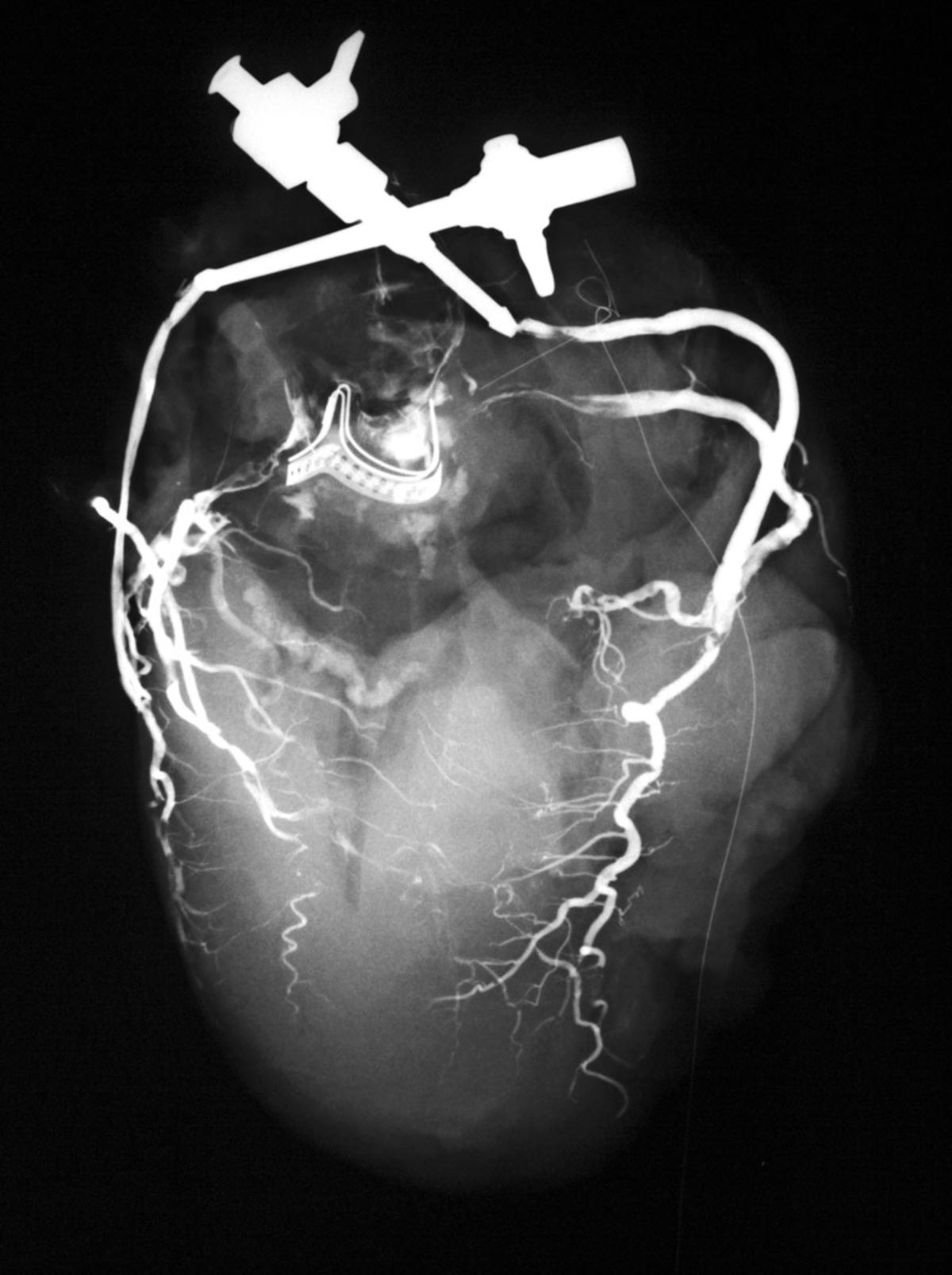
===Diagnostic methods=== | |||
The status of the coronary arteries is typically assessed through imaging techniques. The precise extent of coronary narrowing can be evaluated using coronary angiography during cardiac catheterization. Indirect signs of coronary blood flow can be assessed using tests like ECG (electrocardiogram) or echocardiography. Additional diagnostic procedures include: | |||
* Cardiac CT (computed tomography) | |||
* Cardiac MRI (magnetic resonance imaging) | |||
* | * Myocardial scintigraphy | ||
* | * Intravascular ultrasound (IVUS) | ||
*Myocardial scintigraphy | * Coronary angioscopy | ||
*Intravascular ultrasound (IVUS) | |||
*Coronary angioscopy | |||
==Literature== | ==Literature== | ||
Version vom 17. Oktober 2024, 15:14 Uhr
from Latin: corona - wreath, crown
Definition
Anatomy
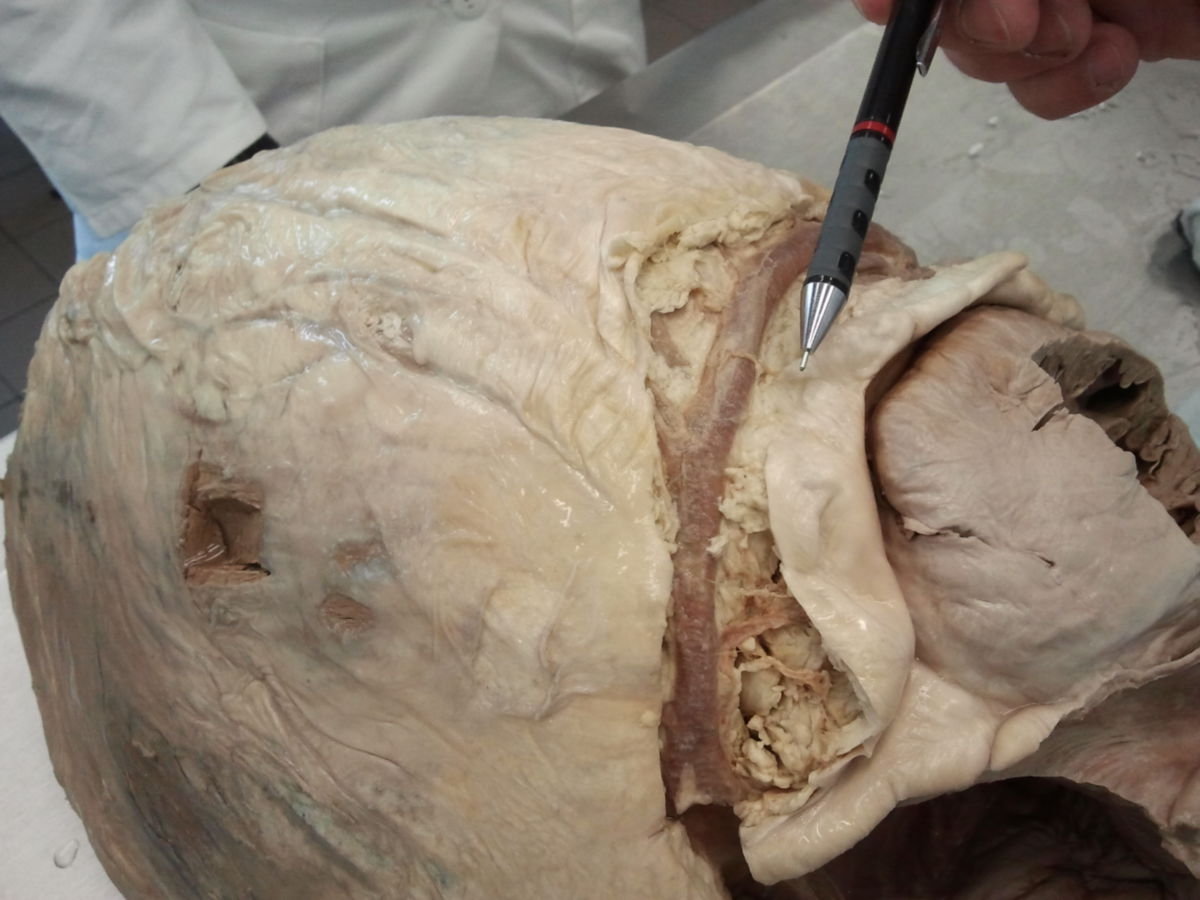
The heart’s blood supply comes from two main coronary arteries: the left coronary artery (LCA) and the right coronary artery (RCA), along with their many branches.
These coronary arteries arise from the ascending part of the aorta, specifically from the right and left aortic sinuses.
Overview of Coronary Artery Branches:
- Left Coronary Artery (LCA, LMCA):
- Circumflex branch (RCX, LCx)
- Atrioventricular branches
- Left marginal branch (left marginal artery)
- Left atrial branch (intermediate artery)
- Left atrial anastomotic branch (globular artery)
- Posterior branch of the left ventricle (posterolateral branch)
- Anterior interventricular branch (LAD, left anterior descending artery)
- Conus branch
- Lateral branch (diagonal branch, anterolateral branch)
- Septal branches (anterior septal branches)
- Circumflex branch (RCX, LCx)
- Right Coronary Artery (RCA):
- Conus branch
- Sinoatrial node branch
- Atrioventricular branches
- Atrial branches
- Right marginal branch
- Posterolateral branch of the right ventricle (RPLD)
- Atrioventricular node branch
- Posterior interventricular branch (RPD, right posterior descending artery)
- Septal branches (posterior septal branches)
This is just one way to classify the coronary artery branches, as individual anatomy often varies depending on the specific type of blood supply to the heart.
Arteria coronaria sinistra
The left coronary artery (LCA) originates from the left aortic sinus, just behind the attachment of the aortic valve. In about 75 % of cases, it is more prominent than the right coronary artery. It travels a short distance between the conus arteriosus and the aorta before dividing into two main branches: the Left Anterior Descending artery (LAD, also known as the anterior interventricular artery) and the Circumflex artery (LCx).
In Bland-White-Garland syndrome, the LCA abnormally arises from the left pulmonary artery rather than the aortic sinus.
Left Anterior Descending Artery (LAD)
The LAD runs downward in the anterior interventricular groove, wraps around the heart's apex, and anastomoses with the posterior interventricular branch of the right coronary artery in the posterior interventricular groove. The LAD gives off the following branches:
- Conus artery: supplies the conus arteriosus.
- Diagonal branch (ramus anterolateralis, ramus diagonalis, RD): supplies the anterior wall of the left ventricle (subject to anatomical variation).
- Septal branches (rami septales anteriores): penetrate the interventricular septum and supply it via superior, inferior, and apical septal branches. A mid-septal branch may also arise, which supplies the anterior papillary muscle of the right ventricle via the moderator band.
Ramus circumflexus
The circumflex artery follows the coronary groove on the left side, running posteriorly toward the diaphragmatic surface of the heart. Its branches include:
- Sinoatrial nodal branch: supplies the sinus node; present in one-third of cases and may arise from either the LCx or right coronary artery.
- Atrioventricular branches: these divide into atrial and ventricular branches, supplying the left atrium and left ventricle.
- Left marginal branch: runs down along the obtuse margin of the left ventricle.
- Intermediate atrial branch: supplies the posterior aspect of the left atrium.
- Atrial anastomotic branch: small branch that forms an anastomosis with branches of the right coronary artery, sometimes supplying the atrioventricular node.
- Posterolateral branch of the left ventricle: supplies the diaphragmatic surface of the left ventricle.
Supply Areas
The areas supplied by the left coronary artery include:
- The anterior wall of the left ventricle (via the LAD and diagonal branches).
- Part of the anterior wall of the right ventricle (via the conus artery and LAD).
- The anterior two-thirds of the interventricular septum (via the septal branches).
- The left atrium (via atrial branches).
- The lateral and posterior walls of the left ventricle, except for the area near the posterior interventricular groove.
Arteria coronaria dextra
The right coronary artery (RCA) arises from the ascending aorta, specifically from the right aortic sinus, located just behind the aortic valve. It travels between the conus arteriosus and the right atrial appendage to reach the right side of the coronary groove (sulcus). From there, it continues along the groove to the diaphragmatic surface of the heart. At the crux of the heart (the point where the coronary sulcus and the interventricular sulcus meet), it gives off its final branch, the posterior descending artery (PDA, also called the posterior interventricular artery), which runs in the posterior interventricular groove toward the apex and connects with the anterior interventricular artery (LAD) from the left coronary artery.
Branches
The RCA gives off the following branches:
- Conus artery: supplies the conus arteriosus and part of the anterior wall of the right ventricle.
- Sinoatrial nodal branch: runs along the front part of the right atrium and usually reaches the sinoatrial node via the terminal groove (sulcus terminalis).
- Atrioventricular branches: these supply the anterior sections of the right atrium and ventricle.
- Atrial branches: supply the lateral parts of the right atrium.
- Right marginal branch: runs along the acute margin (margo acutus) of the right ventricle.
- Posterolateral right ventricular branch: runs parallel to the right marginal branch along the posterior aspect of the right ventricle.
- Atrioventricular nodal branch: arises just before the posterior descending artery and runs through the epicardial fat beneath the atrial septum to supply the atrioventricular (AV) node.
- Posterior descending artery (PDA): the terminal branch of the RCA, which anastomoses with the anterior interventricular artery (LAD) from the left coronary artery.
- Interventricular septal branches: these branches supply the ventricular septum, including the bundle of His and parts of the conduction system.
- Anterior superior septal branches: arise directly from the RCA to supply the upper part of the septum.
- Posterior superior and inferior septal branches: branch off from the posterior descending artery.
Supply area
The right coronary artery supplies the following structures:
- Sinoatrial node (via the sinoatrial nodal branch).
- Atrioventricular node (via the atrioventricular nodal branch).
- Right atrium (via atrial branches).
- Part of the posterior wall of the left ventricle (via the posterolateral right ventricular branch).
- Right ventricle:
- Anterior wall (via conus artery and right marginal branch).
- Lateral wall (via right marginal branch).
- Posterior wall (via the posterior descending artery).
- Ventricular septum: the smaller, posterior portion, including the conduction system (e.g., bundle of His) (via septal branches).
Abbreviations
In the clinical context, the full Latin names are rarely used, but mostly abbreviations. English or Latin abbreviations are commonly used.
| English' - short | Latin - short | Long names' |
|---|---|---|
| RCA | ACD | right coronary artery Arteria coronaria dextra |
| LCA, LMCA | ACS | left coronary artery left m'ain coronary artery Arteria coronaria sinistra |
| LAD | RIVA | left anterior descending coronary artery Ramus interventricularis anterior |
| LCx | RCX | left circumflex coronary artery Ramus circumflexus |
| RPD, R-PDA | RIVP | right posterior descending coronary artery Ramus interventricularis posterior |
| RPLA | RPLD | right posterolateral artery Ramus posterolateralis dexter |
Supply types
The exact areas supplied by the coronary arteries and their branches can vary significantly between individuals. For instance, in about 20 % of cases, the posterior descending artery (PDA) originates from the left coronary artery (LCA), and in 10 % of cases, it arises from both the right and left coronary arteries (codominant supply type).
In roughly 55 % of cases, the heart has a balanced supply type (normal supply type), where the posterior wall of the heart receives blood supply approximately equally from both the right and left coronary arteries.
In 15 to 20 % of cases, the left coronary artery is more dominant (left supply type). In this situation, the circumflex branch (LCx) extends to form the posterior descending artery, which supplies not only the posterior wall of the heart but also a part of the right ventricle and the posterior portion of the interventricular septum.
In the right-dominant supply type (occurring in 15 to 25 % of cases), the right coronary artery (RCA) and particularly its posterolateral branch are more developed. This branch supplies most of the posterior wall of the heart as well as the interventricular septum.
Anatomical variants
Trifurcation
In some individuals, an additional artery arises from the point where the left main coronary artery divides into the LAD (left anterior descending) and the circumflex (LCx). This creates a trifurcation, where a third branch, called the intermediate artery (ramus intermedius), runs along the free wall of the left ventricle toward the apex. This variant is found in about 20 % of the population.
Single coronary artery
A single coronary artery (SCA) is a rare congenital anomaly in which only one coronary artery arises from the aorta to supply the heart. The Lipton classification is used to categorize the different subtypes of this anomaly into three main groups:[1][2]
| group | Course | Name |
|---|---|---|
| I | Follows either the path of a normal right (R) or left (L) coronary artery | RI / LI |
| IIA | Anterior to the pulmonary trunk | RIIA / LIIA |
| IIB | Between the aorta and the pulmonary trunk | RIIB / LIIB |
| IIP | Posterior to the aorta | RIIP / LIIP |
| IIS | Septal course | RIIS / LIIS |
| III | Missing left coronary artery, LAD and RCx arise from the main trunk, starting from the right aortic sinus | RIII |
Physiology
The heart relies on a constant supply of oxygen due to its high workload, making the function of the coronary arteries essential for the heart muscle. The coronary arteries form numerous connections (anastomoses) with each other, but these are not sufficient to create a fully redundant collateral circulation (referred to as "functional end arteries"). If one of the coronary branches becomes blocked, it leads to ischemia (lack of blood supply) in the affected area, followed by necrosis (tissue death) of the heart muscle. During increased cardiac activity, vasodilation (widening) of the coronary vessels is primarily mediated by metabolic by-products, such as carbon dioxide (CO), released by the endothelium.
Clinical significance
Diseases
The most significant disease affecting the coronary arteries is atherosclerosis, which causes narrowing (stenosis) or gradual blockage of the coronary arteries. This condition is known as coronary artery disease (CAD) or coronary heart disease (CHD). Clinically, it manifests as chest pain (angina pectoris), heart attack (myocardial infarction), or heart failure. CHD can be categorized based on the number of coronary vessels affected:
- Single-vessel disease
- Two-vessel disease
- Three-vessel disease
- Left main coronary artery stenosis
Diagnostic methods
The status of the coronary arteries is typically assessed through imaging techniques. The precise extent of coronary narrowing can be evaluated using coronary angiography during cardiac catheterization. Indirect signs of coronary blood flow can be assessed using tests like ECG (electrocardiogram) or echocardiography. Additional diagnostic procedures include:
- Cardiac CT (computed tomography)
- Cardiac MRI (magnetic resonance imaging)
- Myocardial scintigraphy
- Intravascular ultrasound (IVUS)
- Coronary angioscopy
Literature
- Köllner, V. / Berg, G.: Behavioural medicine in the prevention and rehabilitation of cardiovascular diseases. In:Herzmedizin 26 (2009). H.2, PP.69-75.
- Herrmann-Lingen, C.: Depression and coronary heart disease. In: Heart Medicine 26 (2009). H.2, P.76-81.
- Benninghoff, Drenckhahn: Anatomy Volume 2, 16th edition 2004, Elsevier: Urban & Fischer
Sources
- ↑ Lipton et al, Isolated Single Coronary Artery: Diagnosis, Angiographic Classification, and Clinical Significance. Radiology, 1979.
- ↑ Katekaru-Tokeshi et al, Applicability of the Leiden Convention and the Lipton Classification in Patients with a Single Coronary Artery in the Setting of Congenital Heart Disease. Journal of Cardiovascular Development and Disease, 2021