Corpus: Sinus node
Synonyms: sinoatrial node, Keith and Flack node
1. Definition
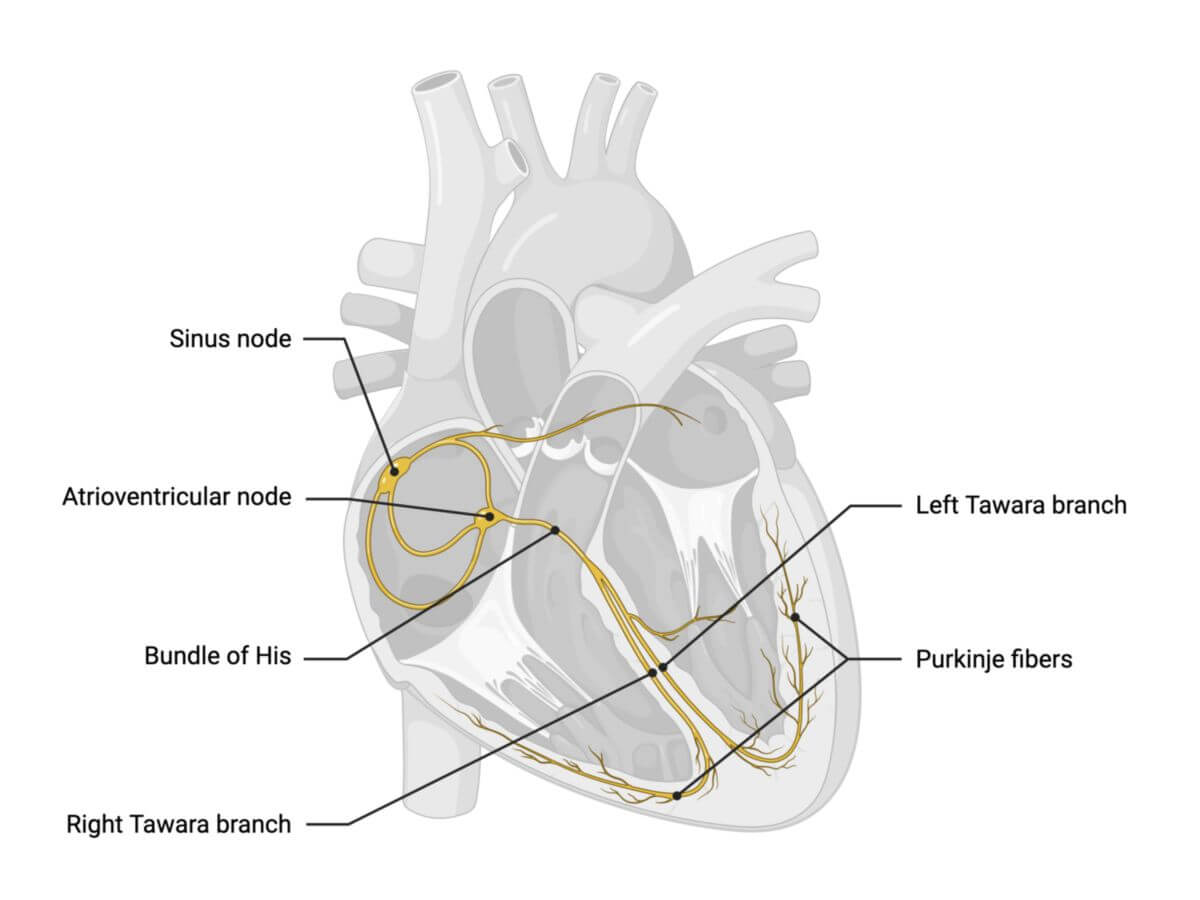
The Sinus node, or sinuatrial node, is the heart's primary pacemaker, responsible for initiating the electrical impulses that regulate the heart rate. It plays a key role in generating and coordinating the heart's excitation signals.
2. Anatomy
The sinus node is a small, comma-shaped structure about 3 mm thick and 10 mm long. It is located subepicardially in the terminal sulcus on the dorsal surface of the right atrium, just below the junction of the superior vena cava. In some cases, it may extend into the right atrial appendage.
The SA node is sometimes described as having three internodal pathways that transmit impulses towards the atrioventricular node:
- Anterior internodal bundle (Bachmann-James bundle)
- Middle internodal bundle (Wenckebach bundle)
- Posterior internodal bundle (Thorel bundle)
The Bachmann bundle, an interatrial bundle, branches from the anterior internodal bundle and transmits impulses to the left atrium.
The existence of distinct internodal bundles remains debated, as they cannot be clearly identified histologically.[1]
The SA node receives blood supply from the ramus nodi sinuatrialis, which typically branches from the right coronary artery and in about 30% of cases from the left coronary artery. The heart rate is regulated by the autonomic nervous system, with sympathetic and parasympathetic (vagus nerve) input to the SA node, modulating heart rhythm.
3. Histology
The histology of the sinus node reveals that it is composed of specialized cardiac muscle cells, primarily P cells and transition cells:
- P cells ("pacemaker" cells) are small, round, and pale. They typically group together and are connected by nexus (connexins 45 and 40) and desmosomes. These cells lack the characteristic striations (intercalated discs) of normal cardiac muscle, and they do not have transverse tubules or a basal lamina. Additionally, they contain only a small number of myofibrils and mitochondria.
- Transition cells are elongated and sometimes branched cardiomyocytes. They contain more myofibrils compared to P cells and serve to connect groups of P cells to one another and to the working myocardium.
4. Physiology
The P cells within the sinus node have a resting membrane potential of approximately -60 mV, which is lower than that of typical cardiomyocytes (-90 mV). The process begins with the hyperpolarization of activated cation channels, leading to a slow influx of sodium ions, referred to as the "I-funny" current, which causes gradual depolarization of the membrane.
When the membrane potential reaches a certain threshold, T-type calcium channels open, allowing a small influx of calcium ions. This, in turn, triggers the opening of L-type calcium channels, resulting in rapid depolarization to approximately +20 mV.
Repolarization and the maintenance of the membrane potential are regulated by potassium channels, which are modulated by the parasympathetic nervous system. M2 acetylcholine receptors on the P cells respond to acetylcholine released by parasympathetic nerve fibers, causing these potassium channels to open. The resulting potassium efflux increases the membrane potential, effectively slowing the heart rate.
Under normal conditions, sinus node cells spontaneously depolarize approximately once per second, initiating electrical excitation that spreads to the surrounding atrial myocardium. This excitation triggers atrial contraction, marking the start of the heart's contraction cycle. The overall heart rhythm is influenced by inputs from the sympathetic nervous system (which accelerates the heart rate) and the parasympathetic nervous system (which slows it down).
Once generated, action potentials from the sinus node are transmitted to the atrioventricular (AV) node within 40 to 80 milliseconds. Conduction occurs particularly rapidly via the crista terminalis.
5. Pathophysiology
In conditions such as sick sinus syndrome, the ability of the sinus node to generate spontaneous electrical stimuli is compromised. When this occurs, the atrioventricular node may take over the role of the primary pacemaker, setting a slower heart rate between 40 and 60 beats per minute.
Additionally, in certain situations like coronary heart disease, the sinus node may depolarize too slowly, leading to sinus bradycardia.
6. Source
- ↑ Sternick et al. Critical Assessment of the Concepts and Misconceptions of the Cardiac Conduction System over the Last 100 Years: The Personal Quest of Robert H. Anderson. Journal of Cardiovascular Development and Disease, January 2021