Corpus: Atrioventricular node
from Latin: atrium - vestibule; ventriculus - small belly
Synonyms: AV node, Aschoff-Tawara node
1. Definition
The atrioventricular node, or AV node for short, is the secondary pacemaker of the heart, playing a key role in regulating heart rate.
2. Anatomy
The AV node is a muscular structure located subendocardially in the right atrium. It is difficult to distinguish macroscopically and is located at the base of the atrial septum, just in front of the junction of the coronary sinus. This region, known as Koch's triangle, is the anatomical landmark where the AV node is located.
2.1. Classification
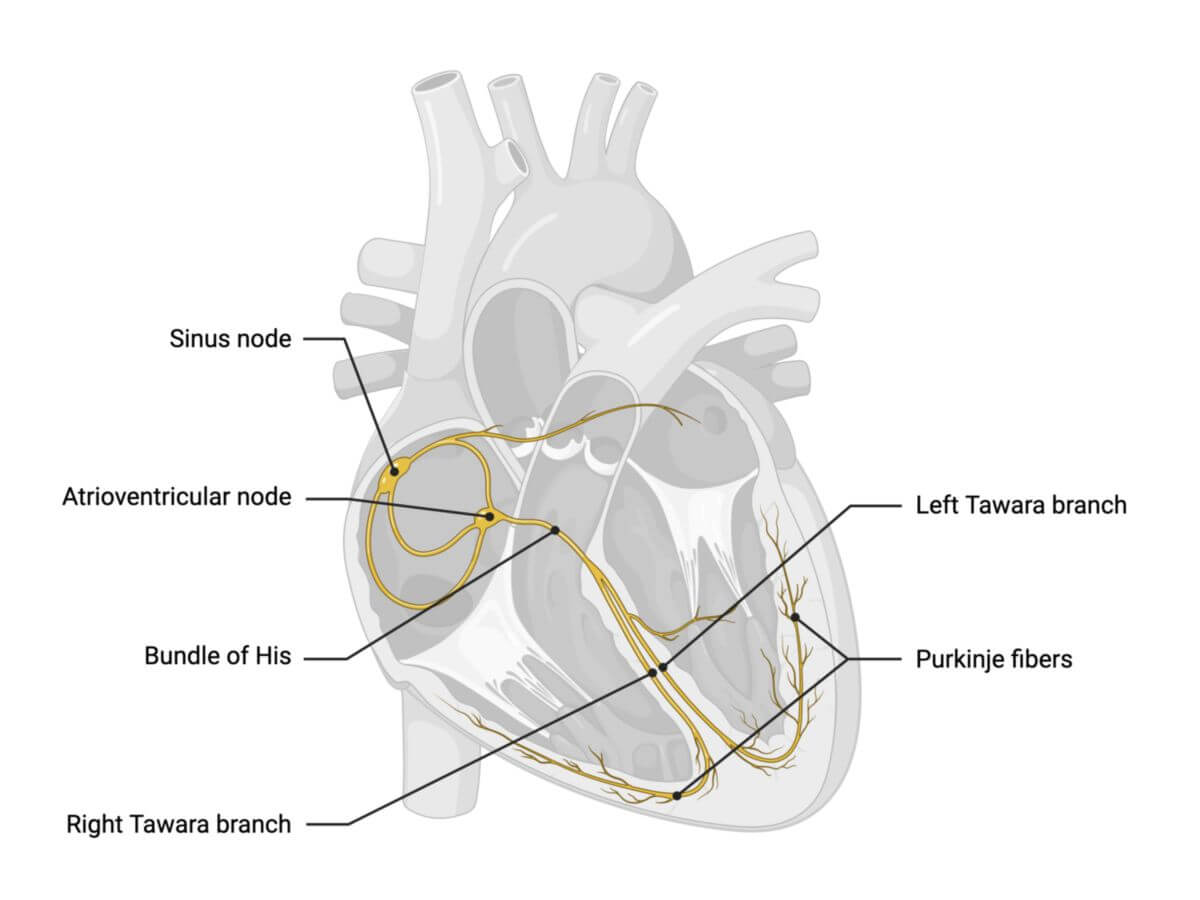
The AV node is divided into three zones:
- Transitional zone: Composed of superior, medial, and posterior atrionodal bundles
- Compact zone: This is the core of the AV node, about 5 mm long, 3 mm wide, and 1 mm thick, located at the tip of the Koch's triangle
- AV bundle zone: This zone continues through the fibrous skeleton of the heart, close to the aortic, mitral, and tricuspid valve and forms the bundle of His.
The bundle of His then bifurcates into the right and left Tawara branches, which give rise to the Purkinje fibres that spread across the endocardial surface of the ventricles.
3. Supply
The AV node receives blood from the right coronary artery (RCA) through the atrioventricular nodal branch, with contributions from the left coronary artery (LCA) via the first septal branch of the left anterior descending artery (LAD). The bundle of His and Tawara branches are perfused by the septal branches of the LAD and lateral branches of the posterior interventricular artery. The AV node is densely innervated by sympathetic and parasympathetic fibres, but the bundle of His and distal conduction system are less autonomically influenced.
4. Histology
The cells of the AV node display heterogeneity in their structure and function. In the proximal transition zone, the cells exhibit an intermediate electrical phenotype, sharing characteristics of both atrial myocytes and cells of the compact zone. The connections at the atrionodal junction can show decremental conduction properties, meaning they slow the transmission of electrical impulses as the stimulation frequency increases.
Moreover, within the AV node, both fast and slow conduction pathways have been identified, likely reflecting functional differences rather than distinct anatomical structures.
The compact zone of the AV node consists of specialised cells known as P cells, which are analogous to the pacemaker cells in the sinus node. These cells contain minimal myofibrils and mitochondria, which limits their contractile ability. The P cells are only weakly connected to each other via nexus (gap junctions made of connexins 45 and 40).
5. Physiology
The AV node functions as the secondary pacemaker of the heart. It receives electrical signals (depolarisations) from the atrial myocardium and transmits them to the ventricles, but with a delay of approximately 60 to 120 milliseconds. This delay, known as the atrioventricular delay (AV time), corresponds to the PQ segment seen on an ECG. The delay mainly occurs in the transition zone of the AV node and serves a critical purpose: it ensures the coordinated contraction of the atria and ventricles. The atria contract slightly earlier than the ventricles, allowing for more effective ventricular filling before they contract.
The AV node also acts as a frequency filter, preventing the transmission of stimuli above a certain frequency. This filtering occurs because of the refractory period of the depolarised heart muscle cells, ensuring that the ventricles don't contract too quickly in response to rapid atrial signals.
The myocytes in the compact zone of the AV node have a resting membrane potential of around -60 mV. Their action potentials differ from regular heart muscle cells in that they have a lower amplitude, a slower phase 0 rise, and a distinctive phase 4 depolarisation. These cells lack the inward potassium current (IK1) and the fast sodium influx (INa). Instead, the calcium influx through L-type calcium channels (ICa-L) is responsible for the phase 0 depolarisation.
Phase 4 depolarisation is governed by the following currents:
- Depolarising currents:
- hyperpolarization-activated cyclic nucleotide-gated channel
- L-type calcium influx (ICa-L)
- T-type calcium influx (ICa-T)
- Repolarising currents:
- Delayed rectifier current (IKr),
- Acetylcholine-controlled current (IKACh)
6. Clinic
The AV node can take over as the primary pacemaker if the sinus node fails, maintaining a heart rate of 40 to 60 beats per minute. When there is a significant delay or failure in the transmission of electrical impulses through the AV node, an AV block occurs, classified into three degrees based on severity.
In some newborns, the AV node is larger and may not remodel properly during infancy, increasing the risk of tachycardia or sudden cardiac death.
Furthermore, abnormal accessory pathways, such as Mahaim and Kent bundles, can bypass the AV node, causing atrioventricular reentry tachycardia (AVRT). If dual conduction pathways exist within the AV node, it can lead to AV nodal reentry tachycardia (AVNRT).