Corpus: Colon
1. Definition
The colon is the longest part of the large intestine, located between the appendix and the rectum.
2. Anatomy
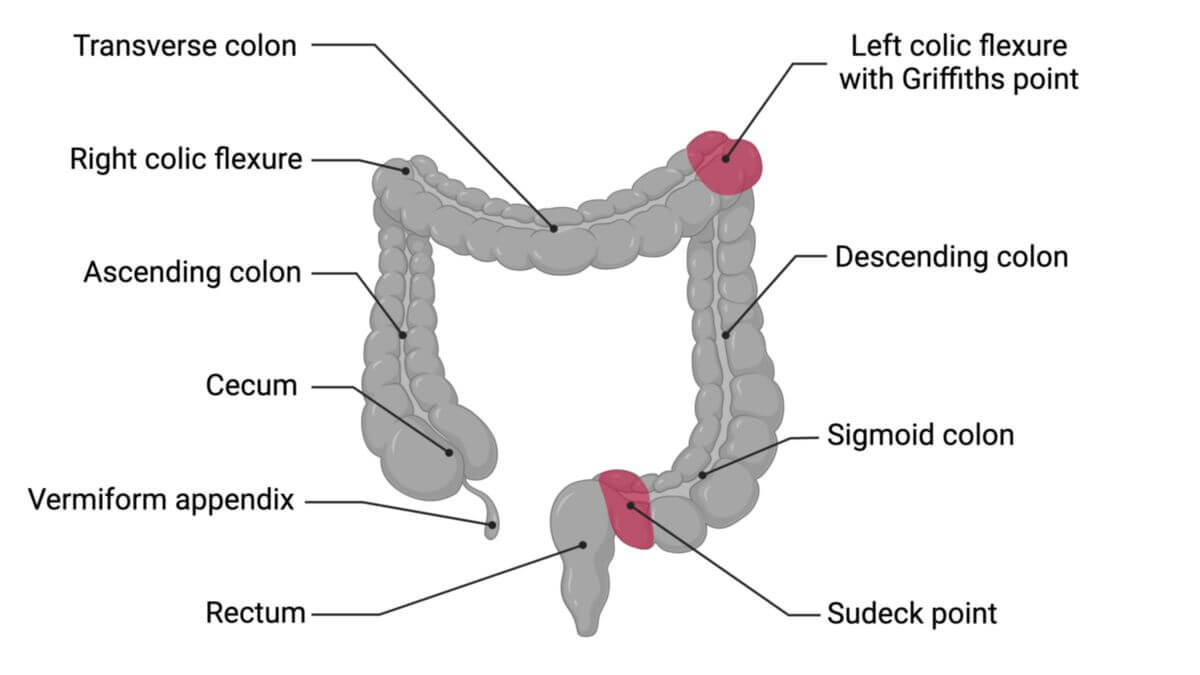
The colon extends from the lower right quadrant of the abdomen, surrounding the small intestine, and is divided into four parts:
The transition from the ascending to the transverse colon is marked by the right colic flexure, while the curve between the transverse and descending colon is called the left colic flexure.
2.1. Location
The ascending and descending colon are retroperitoneal and fused with the posterior abdominal wall via the transverse fascia. The transverse and sigmoid colons are intraperitoneal and have mesenteries, the transverse mesocolon and sigmoid mesocolon, allowing them to be more mobile within the abdominal cavity.
2.2. Dimensions
The colon is the longest segment of the large intestine, measuring approximately 155 cm in women and 166 cm in men.[1] Its diameter varies between 5 and 7 cm.
2.3. Characteristics
The external surface of the colon is distinguished by:
- Haustra: segmental pouches along its length.
- Transverse folds, known as semilunar folds of colon, which correspond to the indentations between the haustr.
- Three longitudinal muscle bands, known as taeniae coli, that aid in identifying the colon during surgery.
- Fat-filled protrusions of subserosal connective tissue, called epiploic appendices.
2.4. Blood supply
The ascending colon is supplied by the ileocolic and right colic arteries, while the transverse colon is primarily supplied by the middle colic artery. All three vessels are branches of the superior mesenteric artery. The descending colon receives blood from the left colic artery, a branch of the inferior mesenteric artery. These arteries form anastomoses, notably the Drummond anastomosis and the Riolan anastomosis, ensuring collateral blood flow. Venous drainage is provided by veins that are named according to the arteries (right, middle, and left colic veins).
2.5. Lymph drainage
The lymph from the ascending colon and the proximal two-thirds of the transverse colon drains into the ileocolic and superior mesenteric lymph nodes, while the distal third of the transverse colon and the sigmoid colon drain into the inferior mesenteric lymph nodes.
2.6. Innervation
The sympathetic innervation of the colon from its beginning to the left colic flexure is provided by the superior mesenteric plexus. From the left colic flexure onward, it is innervated by the inferior mesenteric plexus. Parasympathetic innervation is supplied by the vagus nerve for the proximal colon and by the pelvic splanchnic nerves for the distal colon. The transition between these parasympathetic regions is marked by the Cannon-Böhm point, located in the distal third of the transverse colon.
3. Histology
The structure of the colon wall is largely similar to that of other sections of the intestine. However, unlike other parts, the colon's musculature does not have a continuous longitudinal muscle layer. Instead, it has three distinct bands of longitudinal muscle known as taeniae coli. Typically, the colon lacks intestinal villi but contains a large number of intestinal glands, also called tubular crypts of Lieberkühn. The density of these crypts is estimated at around 100 crypts per mm², which, given the total surface area of the colon (slightly under 1,000 cm²), results in a total of nearly 10 million crypts.
The epithelial lining of the crypts consists of:
- Enterocytes
- Goblet cells responsible for mucin production
- Enteroendocrine cells
- Stem cells
As in other parts of the intestine, the epithelial cells of the colon slough off into the intestinal lumen at the end of their life cycle. These cells are replaced through the continuous division of stem cells located at the base of the crypts. In each crypt, only about 5-6 stem cells are actively dividing, with a division cycle of approximately every 2 to 3 days.
The newly formed cells then migrate along the crypt wall toward the lumen over several days, where they replace the cells that have been shed. This process resembles a conveyor belt of cell renewal.
4. Physiology
The colon plays a key role in absorbing water and electrolytes, thickening the intestinal contents. Peristaltic and antiperistaltic movements mix the contents until they reach a semi-solid consistency. The colon is densely populated with bacteria, forming an individual microbiome that interacts with the immune system and aids in digestion. Bacterial fermentation produces metabolic byproducts, such as vitamin K, which the body can use.
5. Clinic
Important conditions affecting the colon include diarrhea and constipation, along with diseases such as:
- Chronic inflammatory bowel diseases (IBD) like ulcerative colitis and Crohn's disease
- Pseudomembranous colitis
- Colon carcinoma
- Irritable bowel syndrome
- Diverticulitis
In cases of gastrectomy or esophagectomy, parts of the colon may be used for reconstruction of the gastrointestinal tract, a procedure known as colonic interposition.
6. Sources
- ↑ Hounnou G et al: "Anatomical study of the length of the human intestine". Surg Radiol Anat. 24 (5): 290-4 (2002). doi:10.1007/s00276-002-0057-y. PMID 12497219. S2CID 33366428.