Corpus: Lung
1. Definition
The lung is a paired organ used for respiration. It absorbs oxygen from the air we breathe and removes carbon dioxide as an end product of the body's metabolism.
2. Anatomy
2.1. Gross structure
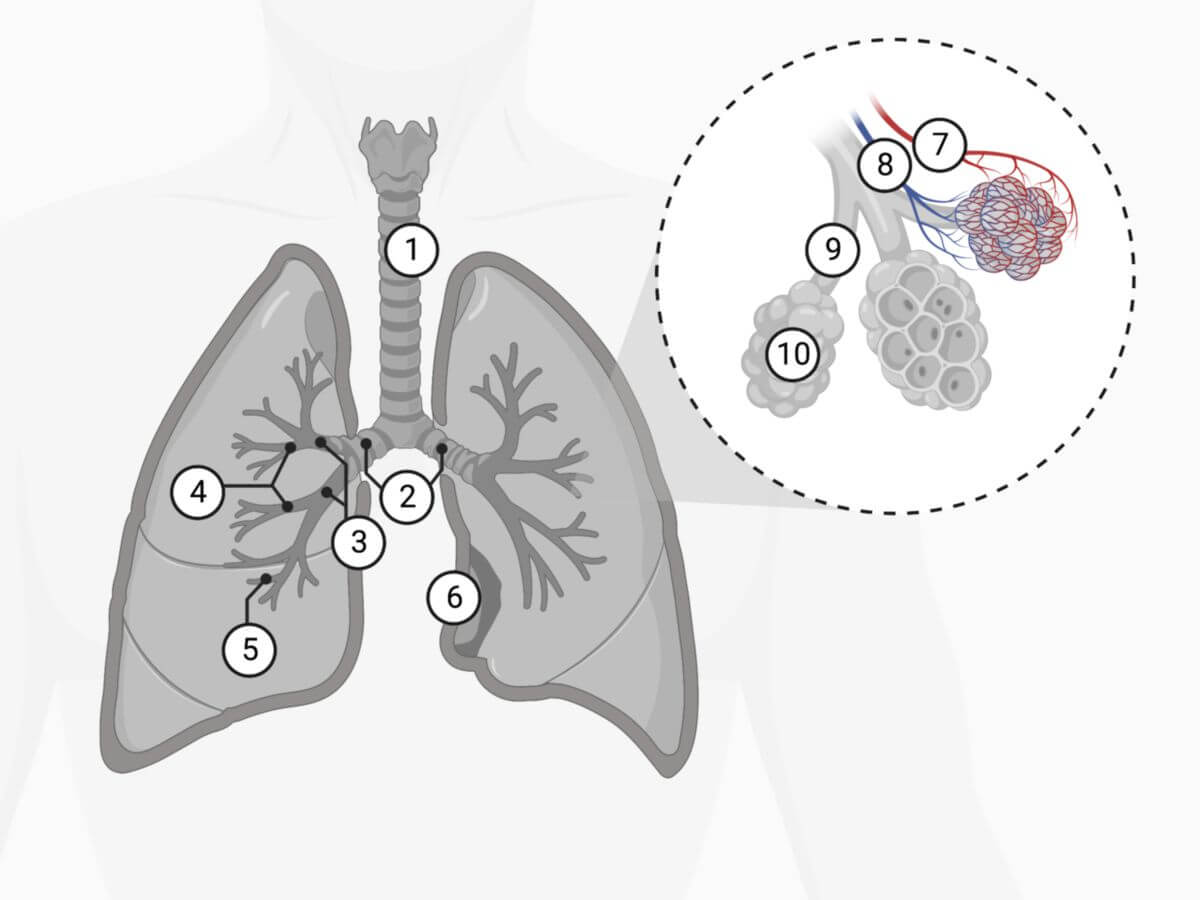
In principle, the lung begins at the pulmonary hilum (hilum pulmonis), lateral to the trachea. This branches in the bifurcation into the two main bronchi (bronchi principales), which enter the hilus together with the pulmonary arteries and the pulmonary veins.
Humans have two lungs that lie on either side of the chest cavity and are separated by the mediastinum. The left lung (pulmo sinister) is divided into two lobes, the right lung (pulmo dexter) into three lobes (lobi pulmonis). The lobes can be further subdivided into 19 lung segments (segmenta bronchopulmonalia), each of which is supplied by a segmental bronchus and a segmental artery. The right lung consists of 10 segments, the left lung of 9 segments. Each segment generally has the shape of a pyramid, with its apex pointing towards the hilum.
2.2. Bronchial tree
The subdivision of the lung is determined by the branches of the bronchi, the bronchial tree. The main bronchi in each half of the lung forms the trunk of the bronchial tree, which splits dichotomously within the lung. The right main bronchus is called the bronchus principalis dexter, the left bronchus principalis sinister.
The main bronchi are divided into the lobar bronchi - on the right into three lobar bronchi: superior, medial and inferior bronchi and on the left into the superior and inferior lobar bronchi. This is followed by a further division into segmental bronchi - 10 on the right and 9 on the left. This is followed by the subsegmental bronchi or lobular bronchi, the bronchioles and finally the terminal bronchioles.
The conductive, air-conducting section of the bronchial tree ends here. This is followed by the section that is used for gas exchange and represents the lung parenchyma. This includes the respiratory bronchioles, the alveolar ducts and the alveolar saccules. The respiratory bronchiole merges into the alveolar duct, which, after further divisions, flows into the final alveolar saccule. The saccule contains the pulmonary alveoli, the actual site of gas exchange. The alveoli are moistened with surfactant to prevent them from collapsing during exhalation.
The latter structures, which originate from a terminal bronchiole, together form a pulmonary acinus. Several of these acini form the structure of the pulmonary lobule, which has a diameter of approximately 2 cm. Characteristic is the macroscopically visible reticular pattern, which represents the boundaries of the pulmonary lobules due to interlobular connective tissue septa and is histologically marked by the dust-laden macrophages lying in the nets.
All bronchi have cartilage, seromucous glands (bronchial glandules) and smooth muscle as structural features in their walls. In the trachea and bronchi, the air-conducting cavities are kept open by cartilage clips. In the smaller bronchi, only island-like cartilage deposits can be seen, but a much thicker layer of smooth muscle. The bronchioles and alveoli no longer contain any cartilage.
It can happen that lung tissue is non-functional because it is not connected to the tracheal tree at all. This is called a pulmonary sequestrum.
2.3. Pleura
On the outside, the lung is covered by the visceral leaf of the pleura (visceral pleura). It extends into the deep fissures (fissurae interlobares). At the pulmonary hilus, the visceral leaf merges into the parietal leaf of the pleura ("pleura"). The pleural duplication caudal to the hilus is known as the pulmonary ligament.
2.4. Vascular supply
The lungs have two circulations, the bronchial and the pulmonary circulation. The bronchial circulation (vasa privata) consists of the bronchial arteries and bronchial veins and serves to supply the lungs themselves. The pulmonary circulation enables gas exchange (vasa publica) and consists of the pulmonary arteries and pulmonary veins.
2.5. Lymphatic drainage
Each lung segment has its own lymphatic drainage, whereby two different lymphatic systems are distinguished:
- deep (or central) network: lymphatic vessels begin in the connective tissue of the terminal bronchioles and accompany the bronchi and arteries. Regional lymph nodes are the bronchopulmonary lymph nodes in the branches of the tracheobronchial tree.
- Superficial (or peripheral) network: Begins in the subserosa and accompanies the intersegmental and interlobar veins in the connective tissue. Regional lymph nodes are the upper and lower tracheobronchial lymph nodes.
Both systems communicate with each other close to the pleura, with the lymph draining from the deep to the superficial system.
See main article: Lymphatic system of the lung
2.6. Innervation
The lungs are innervated by the autonomic nervous system:
- Afferent fibres from stretch receptors in the alveoli and receptors in the bronchi, bronchioles, trachea and larynx run via the vagus nerve.
- Efferent fibres of the vagus nerve run to the smooth muscles and the glands of the tracheobronchial tree. They cause bronchoconstriction, gland secretion and vasodilation.
- Efferent fibres of the sympathetic nervous system cause bronchodilation, vasoconstriction and inhibition of glandular secretion.
3. Histology
3.1. Alveoli
The alveoli are the site of gas exchange (O2 vs CO2) and form a total surface area of approximately 140 m2. The superficial alveolar wall is covered by alveolar epithelium, which harbours two cell types:
- Pneumocytes type 1
- Type 2 pneumocytes (for the production of surfactant).
The polygonal, air-filled spaces (diameter 250 µm) have a capillary network around them and are separated from each other by connective tissue interalveolar septa. These guide the capillaries and thus ensure that the blood-air barrier remains functional. The blood-air barrier can be reduced to three structures:
- Capillary endothelium
- Pneumocytes type 1
- Common basal lamina
3.2. Alveolar macrophages
The alveolar macrophages belong to the monocyte-phagocyte system and eliminate dust particles, germs and dead useless cells on the surface of the alveoli. In addition to the alveoli, alveolar macrophages are found in the terminal, cilia-free airways. After phagocytosis, the alveolar macrophages migrate into the airways equipped with ciliated epithelium, where they are transported with the mucus film. However, the alveolar macrophages can also migrate into the connective tissue of the lung parenchyma, where they either remain and form the lobular pattern or migrate via the lymphatic ducts into the regional lymph nodes.
3.3. Clinal cells
Club cells, formerly Clara cells, are secretory active cells of the distal airways. They secrete antimicrobial and inflammatory proteins. Examples are the surfactant proteins SP-A and SP-D as well as the Clara cell protein CC10.
3.4. Neuroendocrine cells
The neuroendocrine cells of the lung are part of the diffuse neuroendocrine system (DNES). They originate from the neural crest, act as chemoreceptors and secrete hormones such as serotonin, calcitonin and cholecystokinin. They also regulate the development of the lungs.
4. Embryology of the lungs
The future respiratory system is formed as early as the 26th day of pregnancy.
By the end of the first month of pregnancy, five small sacs have already developed from the first anlage. They correspond to the main bronchi of the five lobes of the lungs (two on the left, three on the right). Within a few weeks (up to the 17th week of pregnancy), the entire bronchial apparatus develops through the branching of the cavities.
The first alveoli develop at the end of the pregnancy. The vast majority of alveoli (approx. 80 %) only develop after birth in the first eight months of life.
The lungs fulfil a special function in the womb. As a gland, it forms the amniotic fluid. The fluid fills all parts of the unborn lung. During birth, the lungs are literally squeezed out in the birth canal. This makes it easier for the newborn to fill the lungs with air.
5. Clinic
5.1. Diseases of the lungs
Diseases of the lungs include
- Chronic obstructive pulmonary diseases (COPD, Chronic obstructive pulmonary disease)
- Chronic bronchitis
- emphysema, e.g. with alpha-1-antitrypsin deficiency
- Restrictive lung diseases
- Sarcoidosis
- Pulmonary fibrosis
- Pneumoconiosis (pneumoconiosis)
- Pulmonary oedema
- Atelectasis
- Tuberculosis
- Pneumonia
- Bronchiolitis
- Bronchial carcinoma
5.2. Examination methods
- X-ray thorax
- Thoracic CT
- Lung ultrasound
- Bronchoscopy
6. Weblinks
- Original electron microscope images
- Collection of radiological images of the lung
- Blood-air barrier
- How poor air quality affects the respiratory system] Flash animation by the Union of Concerned Scientists on the destruction of the lungs by ozone and particulate matter